Antibiotic Comparison Tool
Select antibiotics to compare
Choose two or more antibiotics to view their key differences. This tool helps compare indications, advantages, and contraindications based on the article content.
Key Considerations
When choosing between antibiotics, consider: indication, resistance patterns, patient factors (age, allergies, comorbidities), and potential side effects. Always verify local resistance patterns and follow clinical guidelines.
Comparison Results
| Antibiotic | Class | Typical Indications | Key Advantages | Main Drawbacks |
|---|
When doctors need a broad‑spectrum oral antibiotic, Bactrim often lands on the shortlist. But with rising resistance and a growing list of newer agents, patients and clinicians alike wonder how it truly stacks up against the competition. This guide breaks down Bactrim’s chemistry, common uses, and safety profile, then pits it side‑by‑side with the most popular alternatives you’ll see prescribed today.
What Is Bactrim?
Bactrim is a fixed‑dose combination of two antibiotics - sulfamethoxazole and trimethoprim - that work together to block bacterial folic‑acid synthesis. The pairing is known as a sulfonamide‑trimethoprim combo, often abbreviated SMX‑TMP. Because it hits two steps in the same metabolic pathway, it achieves a synergistic effect that’s more potent than either component alone.
The drug was first approved in the United States in 1971 and quickly became a staple for treating urinary‑tract infections (UTIs), certain types of pneumonia, and skin infections caused by susceptible organisms.
Key Pharmacologic Traits
- Sulfamethoxazole is a sulfonamide that mimics para‑aminobenzoic acid (PABA), blocking dihydropteroate synthase.
- Trimethoprim inhibits dihydrofolate reductase, preventing conversion of dihydrofolic acid to tetrahydrofolic acid.
- The standard adult dose for most infections is 800 mg sulfamethoxazole + 160 mg trimethoprim (one double‑strength tablet) every 12 hours.
- Bioavailability exceeds 90 % and the drug is eliminated mainly via the kidneys, making dose adjustment crucial for renal impairment.
When Is Bactrim Typically Used?
Clinical guidelines list Bactrim for:
- Uncomplicated cystitis and acute pyelonephritis caused by E. coli (provided susceptibility is confirmed).
- Community‑acquired pneumonia caused by Streptococcus pneumoniae (especially in patients allergic to penicillin).
- Skin and soft‑tissue infections due to Staphylococcus aureus (including some MRSA strains).
- Prophylaxis against Pneumocystis jirovecii pneumonia (PCP) in immunocompromised patients.
Because it hits a broad range of Gram‑positive and Gram‑negative organisms, Bactrim is often a go‑to when culture data are pending and the physician wants to cover multiple possibilities.
Common Concerns: Side Effects and Contra‑indications
While generally well tolerated, Bactrim carries a few red flags:
- Cutaneous reactions - ranging from mild rash to Stevens‑Johnson syndrome - occur in roughly 1‑2 % of patients.
- Hematologic effects such as leukopenia, thrombocytopenia, or megaloblastic anemia can develop, especially in those with folate deficiency.
- Renal toxicity is a concern in patients with pre‑existing kidney disease; dose reduction is mandatory when creatinine clearance falls below 30 mL/min.
- Pregnancy Category D: the drug crosses the placenta and may cause kernicterus in newborns if given near term.
- Severe hypersensitivity to sulfa drugs is an absolute contraindication.

Alternative Oral Antibiotics Worth Comparing
Below are the most frequently prescribed oral agents that clinicians consider when Bactrim isn’t suitable.
| Drug | Class | Typical Indications | Key Advantages | Main Drawbacks |
|---|---|---|---|---|
| Doxycycline | Tetracycline | Acne, Lyme disease, atypical pneumonia, tick‑borne illnesses | Excellent tissue penetration, anti‑inflammatory properties | Photosensitivity, contraindicated in pregnancy & young children |
| Azithromycin | Macrolide | Community‑acquired pneumonia, chlamydia, otitis media | Once‑daily dosing, good GI tolerance | Potential QT prolongation, rising resistance in S. pneumoniae |
| Amoxicillin | Penicillin | Otitis media, sinusitis, uncomplicated UTIs (when susceptible) | Safe in pregnancy, cheap | Beta‑lactamase resistance, not ideal for MRSA |
| Ciprofloxacin | Fluoroquinolone | Complicated UTIs, prostatitis, GI infections | High oral bioavailability, good for resistant Gram‑negatives | Tendinopathy risk, FDA black‑box warnings for severe side effects |
| Nitrofurantoin | Nitrofuran | Uncomplicated cystitis | Urine‑concentrated, low systemic exposure | Not for pyelonephritis or renal impairment (CrCl <60 mL/min) |
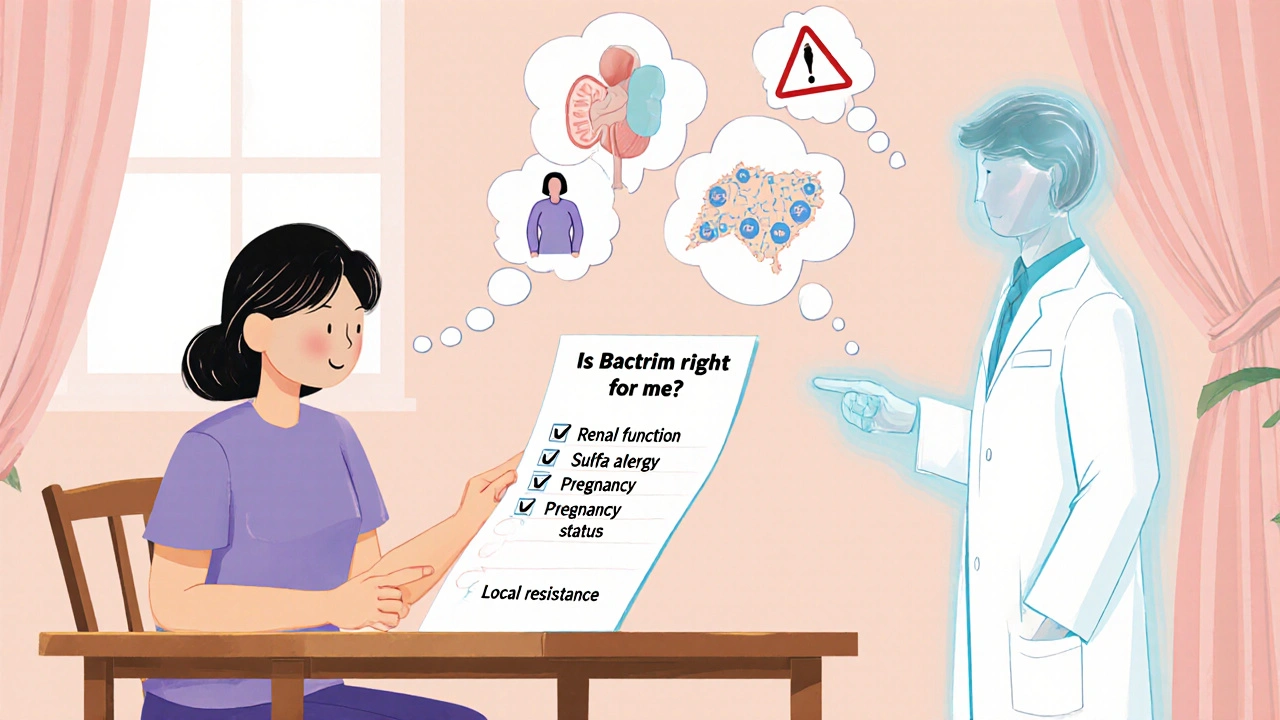
Decision‑Making Framework: When to Choose Bactrim Over Alternatives
Think of antibiotic selection as a balance sheet. Below are the most common criteria you’ll weigh.
- Pathogen Spectrum - Bactrim covers many Enterobacteriaceae and some staphylococci. If you suspect a Gram‑negative UTI and the organism is likely susceptible, Bactrim is a solid first line.
- Local Resistance Patterns - Check your region’s antibiogram. In areas where E. coli resistance to SMX‑TMP exceeds 20 %, agents like nitrofurantoin or fosfomycin may be safer bets.
- Patient Renal Function - Since Bactrim is cleared renally, dose‑adjust or switch to doxycycline or azithromycin for eGFR < 30 mL/min.
- Allergy History - Any sulfa allergy rules out Bactrim. Penicillin‑allergic patients can safely receive Bactrim, but avoid amoxicillin.
- Pregnancy Status - For pregnant women, amoxicillin or nitrofurantoin (second‑trimester) are preferred; Bactrim is avoided.
- Side‑Effect Tolerance - Patients prone to rash or hematologic issues may do better with a macrolide or doxycycline.
- Cost & Accessibility - Bactrim is inexpensive and widely available, which matters for uninsured or low‑income patients.
Practical Guidance for Clinicians
Use the following workflow when you’re faced with a patient who might need Bactrim.
- Confirm the infection type (UTI, pneumonia, skin infection, PCP prophylaxis).
- Review recent culture results or local susceptibility data.
- Check renal function (creatinine clearance) and adjust dose if needed.
- Ask specifically about sulfa allergy and pregnancy status.
- If any red flag appears, move to the next best‑fit alternative from the table above.
- When prescribing, remind patients to stay well‑hydrated, finish the full course, and report any rash or severe GI upset immediately.
Patient‑Centric Tips
Patients often wonder how to tell if Bactrim is the right choice. Here’s a quick cheat‑sheet they can keep at home:
- Good for straightforward bladder infections when you’re not allergic to sulfa.
- Take the dose with a full glass of water; avoid missing doses.
- If you develop a fever, sore throat, or blistering rash, call your doctor right away.
- Don’t use it if you’re pregnant or trying to become pregnant unless your doctor says it’s absolutely necessary.
- Keep an eye on the color of your urine - a sharp change could signal a kidney issue.
Frequently Asked Questions
Is Bactrim safe for children?
Bactrim can be used in children over 2 months of age for specific infections, but dosing must be weight‑based and closely monitored for bone‑marrow suppression.
How quickly does Bactrim start working?
Patients often feel symptom relief within 48‑72 hours, although the full course (usually 5‑7 days) should be completed to prevent relapse.
Can I take Bactrim with other medicines?
Bactrim interacts with warfarin, certain diabetes drugs, and some NSAIDs. Always list all current meds to your prescriber.
Why do some doctors prefer nitrofurantoin for cystitis?
Nitrofurantoin concentrates in the urine, achieving high local levels while exposing the rest of the body to minimal drug, reducing systemic side‑effects and resistance pressure.
What should I do if I miss a dose?
Take the missed dose as soon as you remember unless it’s almost time for the next one. In that case, skip the missed dose and resume your regular schedule - don’t double‑up.
Bottom Line
Bactrim remains a workhorse for many common infections thanks to its broad coverage, low cost, and oral convenience. However, its sulfa component, renal clearance, and pregnancy warnings mean it isn’t a universal fit. By weighing pathogen likelihood, local resistance data, patient comorbidities, and safety concerns, clinicians can decide when Bactrim shines and when an alternative like doxycycline, azithromycin, or nitrofurantoin provides a better balance of efficacy and risk.

jagdish soni
Ah the grand theater of antibiotics where Bactrim claims a venerable seat yet often drifts into obscurity. Its sulfa‑trimethoprim duet dances on folate pathways like an alchemist seeking aureate cure. Beware though the specter of rash and renal strain that haunts even the most gallant of prescriptions.
parth gajjar
The lament of a patient bound to sulfa allergies is a mournful aria that echoes through clinic halls. When the winds shift, clinicians must summon alternatives lest the chorus falters. Doxycycline rises with a fierce crescendo of tissue reach while azithromycin whispers soothing once‑daily ease.
Maridel Frey
Choosing an appropriate oral antibiotic requires a systematic assessment of the infection site, likely pathogens, and patient-specific factors.
Bactrim remains a valuable option for uncomplicated urinary‑tract infections caused by susceptible Escherichia coli strains, provided renal function is adequate.
Its dual mechanism-sulfamethoxazole inhibiting dihydropteroate synthase and trimethoprim blocking dihydrofolate reductase-produces a synergistic bacteriostatic effect.
However, clinicians must verify sulfa hypersensitivity before prescribing, as cross‑reactivity can precipitate severe cutaneous reactions.
In cases of community‑acquired pneumonia where atypical organisms predominate, macrolides such as azithromycin or tetracyclines like doxycycline often achieve superior coverage.
Azithromycin offers the convenience of once‑daily dosing and a favorable gastrointestinal tolerance profile.
Conversely, its potential to prolong the QT interval mandates caution in patients with existing cardiac arrhythmias.
Doxycycline provides excellent intracellular penetration, making it suitable for atypical pathogens, but it is contraindicated in pregnancy and early childhood due to effects on bone growth.
Fluoroquinolones such as ciprofloxacin deliver high oral bioavailability and potent activity against resistant Gram‑negative organisms, yet the FDA black‑box warnings for tendinopathy and vascular events limit their routine use.
Nitrofurantoin remains a first‑line agent for uncomplicated cystitis because it concentrates in the urinary tract while minimizing systemic exposure.
Renal impairment, however, precludes its use when creatinine clearance falls below 60 mL/min.
Amoxicillin, a beta‑lactam, is generally safe in pregnancy and well‑tolerated, but beta‑lactamase producing organisms may render it ineffective without a beta‑lactamase inhibitor.
When faced with methicillin‑resistant Staphylococcus aureus (MRSA), agents such as clindamycin or linezolid should be considered over Bactrim if local susceptibility data suggest resistance.
Prophylaxis against Pneumocystis jirovecii pneumonia in immunocompromised hosts continues to rely on Bactrim due to its proven efficacy and cost‑effectiveness.
Nevertheless, folate supplementation may be warranted to mitigate the risk of megaloblastic anemia in long‑term users.
Ultimately, the decision matrix balances antimicrobial spectrum, patient comorbidities, resistance patterns, and safety considerations to arrive at the most judicious therapy.
Madhav Dasari
Hey folks, let’s shine a light on the fact that no antibiotic is a magic bullet, but Bactrim can still be a hero in the right storyline. When the culture results are pending, its broad‑spectrum cover buys you time, and that’s a win‑win for both doctor and patient. Remember to check renal function and allergy history-those are the plot twists you don’t want.
DHARMENDER BHATHAVAR
Bactrim is effective for cystitis and PCP prophylaxis but requires dose adjustment in renal impairment.
ashanti barrett
While the concise summary hits the nail, it’s crucial to also note the hematologic risks-leukopenia and thrombocytopenia can emerge, especially in folate‑deficient patients, so monitoring CBCs is advisable.
Leo Chan
Great points! If you’re dealing with a skin infection and Bactrim isn’t an option, doxycycline can swoop in with anti‑inflammatory perks, and azithromycin offers that easy‑once‑daily regimen we all love.
Latasha Becker
Contrary to the prevailing narrative that positions Bactrim as a first‑line stalwart, pharmacodynamic profiling reveals its post‑antibiotic effect is comparatively modest, rendering it suboptimal for high‑inoculum infections where time‑dependent killing is paramount; thus, agents with superior %T>MIC, such as β‑lactams, should be prioritized.
Kevin Sheehan
In the grand dialectic of antimicrobial stewardship, each prescription is a thesis, each resistance pattern a antithesis, and the synthesis is the judicious selection that transcends dogma; Bactrim, with its dual‑target mechanism, embodies a dialectical balance, yet must be wielded with the rigor of a seasoned rhetorician.
Jay Kay
Honestly, Bactrim feels outdated.