When a patient walks into the ER with shortness of breath, chest tightness, or swollen ankles, the question isn’t just what’s wrong-it’s how fast can we rule out heart failure? That’s where NT-proBNP blood testing comes in. It’s not just another lab order. For clinicians, it’s often the fastest, most reliable way to tell if someone’s heart is under stress-or if their symptoms are coming from something else entirely.
Why NT-proBNP Is the Go-To Test for Suspected Heart Failure
NT-proBNP stands for N-terminal pro-B-type natriuretic peptide. It’s a protein released by the heart when the ventricles are stretched from too much pressure or fluid. Think of it like a distress signal. When the heart is struggling, it releases more of this marker into the bloodstream. The test measures how much is there-and that number tells you a lot, fast.
Unlike imaging tests like echocardiograms-which can take days to schedule and cost thousands-NT-proBNP results are often back in under an hour. In emergency departments across the UK and US, it’s now standard practice to order this test within 30 minutes of a patient arriving with suspected heart failure. Why? Because a level below 300 pg/mL rules out acute heart failure with 98% accuracy. That’s not a guess. That’s science backed by over 20 years of data from the European Society of Cardiology and the American College of Cardiology.
Here’s what that means in real life: An 82-year-old with COPD comes in wheezing and swollen. An echocardiogram might cost $3,000 and take weeks. But if their NT-proBNP is 120 pg/mL? You don’t need it. Their breathing trouble is likely from a lung infection, not heart failure. You treat the lungs, avoid unnecessary hospitalization, and save the system money.
When Exactly Should You Order It?
Not every patient with fatigue or swelling needs this test. Ordering it blindly leads to confusion, not clarity. Here’s when it makes sense:
- Acute dyspnea (sudden shortness of breath)-especially in patients over 50, or those with known heart disease, hypertension, or diabetes.
- New-onset edema-ankle swelling that doesn’t improve with elevation or diuretics.
- Unexplained fatigue or reduced exercise tolerance-particularly when combined with a history of heart attack or atrial fibrillation.
- Patients being evaluated for heart failure in primary care-NICE guidelines recommend NT-proBNP as the first-line test before referring to cardiology.
Don’t order it for routine checkups. Don’t order it for asymptomatic patients with no risk factors. Medicare data shows 18% of tests are ordered in people with no symptoms-and that’s where overuse starts. Starting January 2025, CMS will require prior authorization for NT-proBNP tests in low-risk, asymptomatic patients. It’s not about cutting costs-it’s about cutting noise.
How to Interpret the Numbers-It’s Not Just One Cutoff
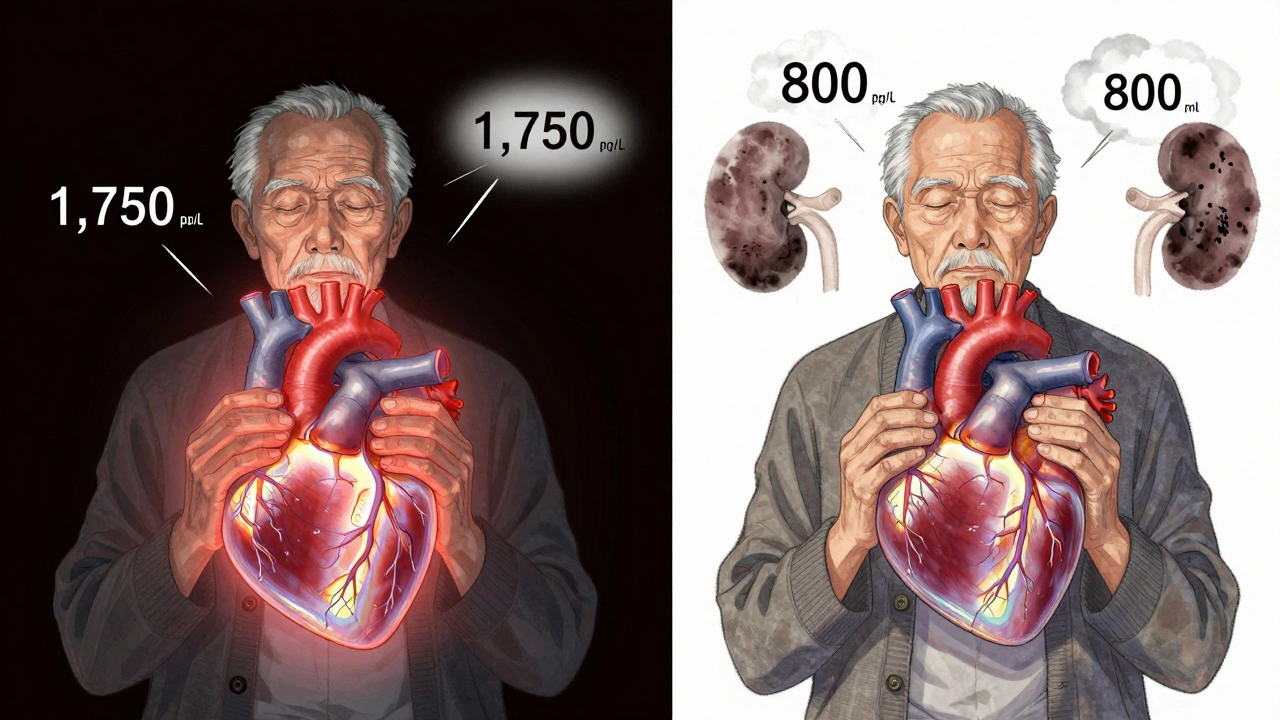
Here’s where things get tricky. NT-proBNP levels naturally rise with age. A 75-year-old with a level of 800 pg/mL might be perfectly fine. A 45-year-old with the same level? That’s a red flag.
The European Society of Cardiology gives clear age-based cutoffs for ruling out heart failure:
- Under 50 years: < 450 pg/mL
- 50-75 years: < 900 pg/mL
- Over 75 years: < 1,800 pg/mL
These aren’t arbitrary. They’re based on population studies tracking outcomes over decades. But here’s the catch: if the patient has chronic kidney disease (CKD), those numbers go up. In stage 3-4 CKD, NT-proBNP levels can be 28-40% higher than normal-even without heart failure. That’s because the kidneys clear the peptide. When they’re weak, it builds up.
So for CKD patients, use a modified cutoff: < 1,200 pg/mL to rule out heart failure. Don’t rely on the standard numbers. Misinterpreting this is one of the top reasons clinicians get burned.
Obesity also lowers NT-proBNP levels-by 25-30% for every 5-point increase in BMI. So a 300 pg/mL result in a very obese patient might still be too high. Always consider body weight.
NT-proBNP vs. BNP: Why One Dominates
You might hear doctors talk about BNP instead. Both are natriuretic peptides, but NT-proBNP is now the preferred test in most settings. Why?
- Stability: NT-proBNP lasts longer in the blood-up to 2 hours versus BNP’s 20 minutes. That means you can transport samples without rushing. No more panic if the lab is backed up.
- Accuracy: Studies show NT-proBNP has a slightly higher diagnostic accuracy (AUC 0.91 vs. 0.88) and better correlation with heart function seen on echo.
- Market dominance: In the US, 68% of all natriuretic peptide tests ordered are NT-proBNP. Roche’s Elecsys assay is used in 73% of labs.
BNP is still useful in some cases-like when you need rapid point-of-care testing. But for most hospitals and clinics, NT-proBNP is the gold standard.
Real-World Pitfalls and How to Avoid Them
Even with clear guidelines, mistakes happen. Here are the most common missteps-and how to fix them:
- Ordering it for atrial fibrillation without context: AFib alone can raise NT-proBNP. Don’t assume heart failure. Look for other signs: elevated jugular venous pressure, crackles in lungs, S3 gallop.
- Ignoring renal function: Always check eGFR. If it’s below 60, adjust your cutoffs.
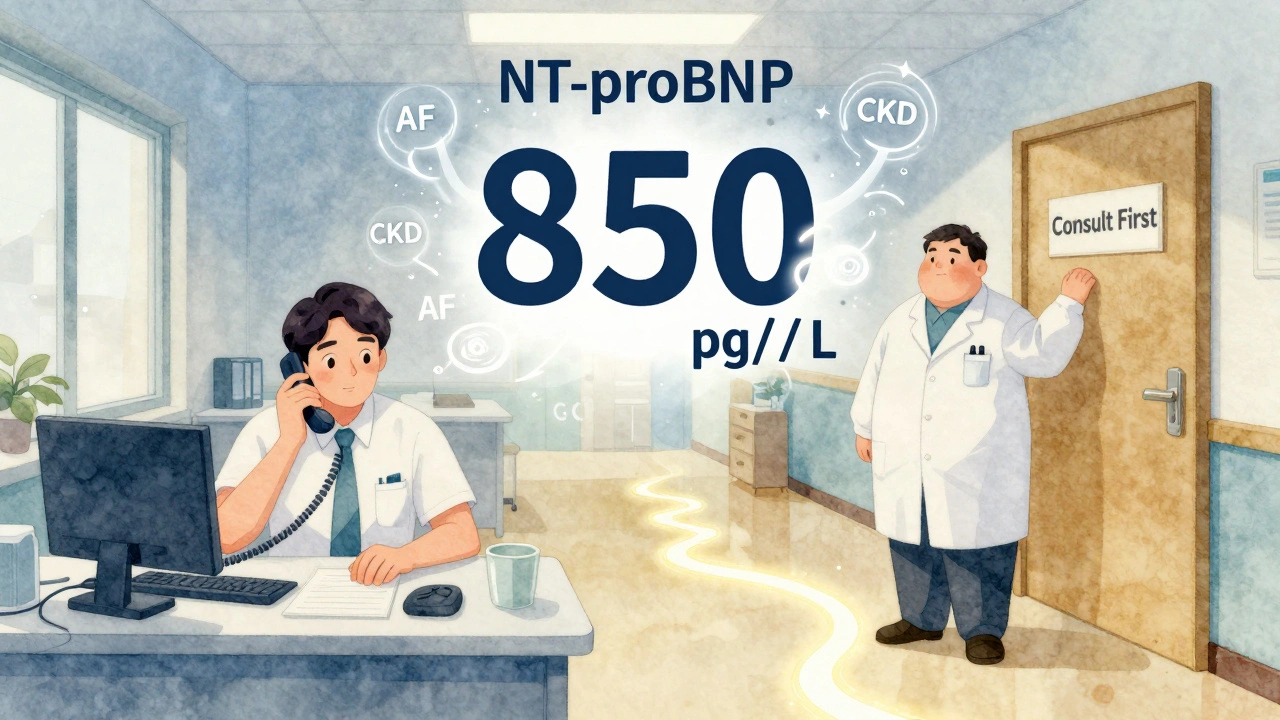
- Using the test as a standalone: NT-proBNP tells you about cardiac stress, not the cause. Combine it with clinical exam, ECG, chest X-ray, and kidney function. A level of 1,500 pg/mL in a 78-year-old with CKD and AFib? That’s ambiguous. That’s when you call the Heart Failure Society’s interpretation hotline-or refer to cardiology.
- Not documenting the reason: If you order it, write why. “Suspected acute heart failure” or “differential diagnosis: COPD vs. CHF.” That helps future providers and audits.
One cardiologist in Nottingham told me: “I used to order echos for everyone with breathlessness. Now I order NT-proBNP first. If it’s low, I move on. If it’s high, I know I need to dig deeper. It’s changed how I practice.”
The Future: Point-of-Care and New Guidelines
Technology is catching up. In 2023, the FDA cleared Roche’s Cobas h 232-a point-of-care device that gives NT-proBNP results in 12 minutes. That’s faster than drawing blood in some ERs. It’s already being rolled out in UK urgent care centers and large GP practices.
And the guidelines are expanding. The 2024 ACC/AHA/HFSA update (released September 2024) now recommends NT-proBNP testing for risk stratification in patients with acute coronary syndrome. Why? Because even after a heart attack, high NT-proBNP levels predict higher risk of death or rehospitalization. It’s no longer just for heart failure-it’s becoming a general marker of cardiac strain.
But here’s the bottom line: NT-proBNP isn’t magic. It doesn’t replace clinical judgment. It enhances it. Used right, it cuts down unnecessary tests, reduces hospital stays, and gets patients the right care faster. Used wrong? It creates false reassurance-or unnecessary panic.
What Clinicians Are Saying
A 2023 Medscape survey of 1,247 cardiologists found 89% call NT-proBNP “essential.” Seventy-six percent say it’s prevented at least one unnecessary hospital admission in the past month.
One GP wrote on a medical forum: “I had a 70-year-old woman with fatigue and ankle swelling. Her NT-proBNP was 210. I told her it was likely just aging and gave her a walking plan. Six months later, she came back saying she’s hiking again. No echo. No meds. Just a simple blood test.”
Another said: “My biggest headache? When the result is 850 in an elderly patient with AFib and CKD. Is it heart failure? Or just a perfect storm of aging and kidney decline? That’s where experience matters. That’s why we need training-not just tests.”
The solution? Use the tools. Use the guidelines. And when in doubt-consult.
The Heart Failure Society of America runs a free NT-proBNP Interpretation Hotline (1-800-NT-PROBNP). It gets 1,200 calls a month. Ninety-four percent of callers say it helped them make the right call. That’s not just a service-it’s a lifeline.
Final Takeaway
NT-proBNP testing isn’t optional anymore. It’s standard. But it’s not a reflex. It’s a tool-powerful, precise, and only as good as the person using it.
If you’re seeing a patient with possible heart failure, order it early. Know the age- and kidney-adjusted cutoffs. Don’t interpret it alone. And never let a number replace a clinical picture.
Because in medicine, the best tests don’t just give answers. They give clarity. And sometimes, that’s all you need to make the right decision-fast.
What is NT-proBNP and why is it tested?
NT-proBNP is a protein released by the heart when its ventricles are stretched due to increased pressure, often from heart failure. The blood test measures this marker to help diagnose or rule out heart failure quickly. It’s preferred over BNP because it’s more stable, easier to measure accurately, and has better diagnostic performance in most clinical settings.
When should a clinician order an NT-proBNP test?
Order NT-proBNP when a patient presents with symptoms like sudden shortness of breath, unexplained fatigue, or swelling in the legs-especially if they’re over 50 or have risk factors like high blood pressure, diabetes, or prior heart disease. It’s recommended by NICE and ESC guidelines as the first-line test for suspected heart failure in emergency and primary care settings.
What NT-proBNP level rules out heart failure?
The rule-out threshold is 300 pg/mL for acute heart failure, but age-adjusted cutoffs are more accurate: under 450 pg/mL for patients under 50, under 900 pg/mL for ages 50-75, and under 1,800 pg/mL for those over 75. For patients with chronic kidney disease, use a modified cutoff of under 1,200 pg/mL.
Can NT-proBNP be elevated without heart failure?
Yes. NT-proBNP levels rise with age, kidney disease, atrial fibrillation, and even severe lung infections. Obesity can lower levels. That’s why interpretation must always include clinical context-never rely on the number alone. A high result doesn’t confirm heart failure; it signals cardiac stress that needs further investigation.
Is NT-proBNP testing covered by insurance?
Yes. In the US, Medicare reimburses approximately $18.42 per test as of 2023. In the UK, it’s routinely covered under NHS pathology services. However, starting January 2025, Medicare will require prior authorization for NT-proBNP tests ordered in asymptomatic or low-risk patients to reduce inappropriate use.
How long does it take to get NT-proBNP results?
In hospital labs, results typically take 47 minutes on average. With newer point-of-care devices like the Roche Cobas h 232, results can be available in as little as 12 minutes, making it feasible for use in emergency departments and urgent care centers.
What’s the difference between NT-proBNP and BNP?
Both are biomarkers of heart stress, but NT-proBNP is the inactive fragment with a longer half-life (60-120 minutes vs. 20 minutes for BNP), making it more stable in blood samples. NT-proBNP also has slightly higher diagnostic accuracy and is less affected by short delays in testing. As a result, NT-proBNP is now the preferred test in most clinical settings.
Can NT-proBNP predict outcomes in heart failure?
Yes. Higher NT-proBNP levels strongly correlate with worse prognosis-increased risk of hospitalization, cardiovascular death, and disease progression. It’s now used not just for diagnosis but also for risk stratification, especially after heart attacks or in patients with advanced heart failure. Trends over time (serial testing) are often more telling than a single value.


Louis Llaine
So let me get this straight-we’re now paying $18 to avoid an echo that costs $3k? Sounds like a win until you realize half the time the number means nothing because the patient’s got CKD, obesity, and AFib all at once. Just give me a stethoscope and a gut feeling.
Kyle Oksten
This test isn’t magic-it’s a filter. The real skill isn’t ordering it, it’s knowing when to stop. Medicine isn’t about chasing numbers. It’s about understanding the person behind the lab result. If you’re treating the biomarker instead of the patient, you’ve already lost.
Sam Mathew Cheriyan
lol did u know the gov t is secretly using nt-probnp data to track how many old people are dying? theyre building a death clock. also my cousin in india got his test done and the lab said his level was 8000 but he was fine. maybe its a conspiracy. or maybe labs just suck. 🤔
Ernie Blevins
This is why docs are useless. You order a test, get a number, and then you still don’t know what’s wrong. Why not just give everyone a CT? At least then you see the problem. This is just wasting time and money.
Ted Rosenwasser
The fact that you need a hotline to interpret a biomarker should tell you something. We’ve outsourced clinical reasoning to a spreadsheet. This isn’t medicine-it’s algorithmic triage with a white coat. 📊
Ashley Farmer
I’ve seen so many elderly patients scared silly because their NT-proBNP was 'high.' But when we sat down, talked about their daily life, their meds, their sleep-it turned out they were just tired from caring for their spouse with dementia. The number didn’t lie. But it didn’t tell the whole story either. Always listen first.
Jennifer Anderson
i was reading this and thought wow this is so useful but then i remebered my aunt got her test done and the doc just said 'oh its high' and sent her to cardio and she ended up with a 3 day hospital stay for nothing. maybe we need more training for docs not just more tests? 🤷♀️
Kurt Russell
THIS IS THE FUTURE. Imagine walking into urgent care, getting a finger prick, and in 12 minutes you know if your heart is in trouble or not. No waiting. No guesswork. No panic. This isn’t just a test-it’s a revolution. And it’s here. Let’s not waste it. 🚀
Kyle Flores
I’ve been using this test for years. The biggest thing I’ve learned? Don’t trust the number if the patient looks fine. I had a guy with a 1,700 result who jogged 5 miles every morning. Turns out he had stage 3 CKD and just never told anyone. We didn’t treat heart failure-we treated his kidneys. Context is everything.
Ryan Sullivan
The notion that NT-proBNP is a 'gold standard' is a dangerous myth perpetuated by Roche’s marketing team. It’s a surrogate marker with significant confounders. To rely on it without integrating clinical context is not evidence-based medicine-it’s lazy pharmacoeconomics dressed up as innovation.
Wesley Phillips
So you’re telling me we’ve got a blood test that can tell if your heart is stressed… but you need a PhD to read it? And if you’re fat or old or have kidney issues? Forget it. Just give me a magic wand already 😅
Olivia Hand
I’m curious-how many of these 'high' results in elderly patients with CKD are actually just normal aging? We treat biomarkers like they’re diagnoses, but what if they’re just… signatures of time? Is that a disease? Or just biology?
Desmond Khoo
This is why I love medicine. A simple blood draw can save someone from a week in the hospital. No fancy machines. No waiting. Just science doing its job. Keep it simple. Keep it smart. 🙌
Jane Quitain
i just had my dad get this test done and the doc said 'its normal' and we were so relieved but then he got worse a week later… so i dont know if the test is wrong or if we just got lucky. maybe we need more than one test? 🥺
Nancy Carlsen
I work in a rural clinic where we don’t have echos for months. NT-proBNP is our lifeline. One woman came in with swelling and fatigue-her level was 210. I told her it was likely just aging. Six months later, she sent me a photo of her hiking with her grandkids. No meds. No echo. Just a test and trust. That’s why I do this.