For many people, a persistent cough that won’t go away isn’t just annoying-it’s a warning sign. If you’ve been coughing up mucus for months, or even years, and it keeps coming back every winter, you might be dealing with chronic bronchitis. It’s not just a bad cold that lingers. It’s a real, long-term lung condition that affects breathing, energy, and daily life. And the good news? You can take control of it-even if you’ve been smoking for decades.
What Exactly Is Chronic Bronchitis?
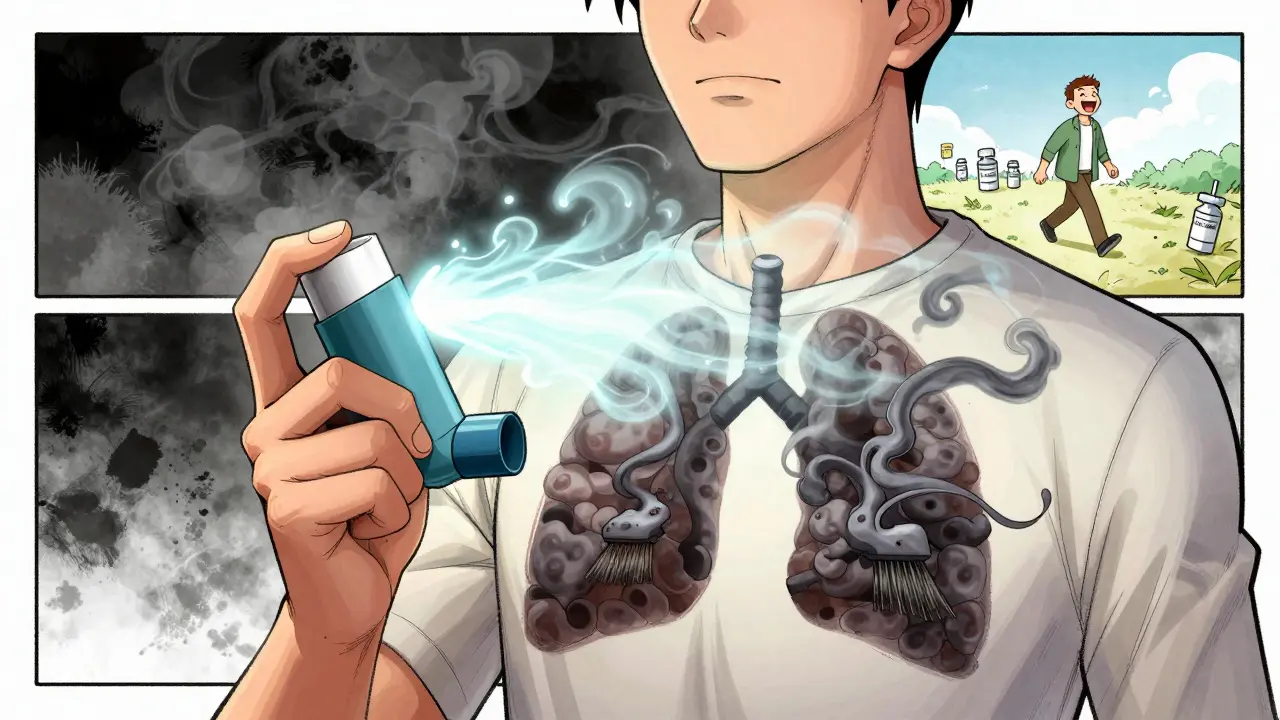
Chronic bronchitis isn’t just a cough. It’s defined by a productive cough-meaning you’re bringing up mucus-that lasts at least three months a year, for two years in a row. This isn’t something you shake off after a week. It’s inflammation in the airways that makes them produce too much mucus, which then blocks the flow of air. Over time, this leads to shortness of breath, especially when you walk up stairs or carry groceries. It’s one of the two main forms of COPD (chronic obstructive pulmonary disease), along with emphysema. About 10 million Americans have been diagnosed, but many more may be undiagnosed because they think it’s just "a smoker’s cough." The truth? It’s not normal. And it gets worse without action.Why Smoking Is the Biggest Culprit
Over 90% of people with chronic bronchitis have smoked-or still do. Smoking doesn’t just irritate your lungs; it destroys the tiny hairs (cilia) that normally sweep mucus out of your airways. Without them, mucus builds up, bacteria thrive, and infections become common. Even if you quit decades ago, the damage can still show up now. But here’s something important: not every smoker gets chronic bronchitis. Only about 15% of smokers develop serious airway disease. That means genetics, environment, and how long you smoked all play a role. Still, if you’re a current smoker, your risk is 42% over 30 years. If you quit, that drops to 26%. That’s not a small difference-it’s life-changing.What Symptoms Should You Watch For?
The cough and mucus are the hallmarks, but they’re not the only signs. Many people don’t realize how much their daily life has changed until they stop and think about it:- Shortness of breath during light activity (82% of patients experience this)
- Chest tightness or discomfort (68% in moderate to severe cases)
- Wheezing when breathing out (57% of cases)
- Constant fatigue (73% report feeling worn out even after resting)
- Frequent lung infections that make symptoms worse
Smoking Cessation: The Only Treatment That Actually Slows the Disease
Here’s the hard truth: no pill, inhaler, or therapy can stop chronic bronchitis from progressing like quitting smoking can. Every major medical group-from the American Lung Association to the Global Initiative for Chronic Obstructive Lung Disease (GOLD)-says the same thing: stop smoking, and you slow the damage. Studies show that people who quit smoking after diagnosis have 60% slower disease progression than those who keep smoking. That’s not just a better quality of life-it means living longer. One 58-year-old patient from HealthUnlocked said, “After six months of quitting and doing rehab, I could walk to the end of my street without stopping. I hadn’t done that in three years.” But quitting isn’t easy. Most people try multiple times before they succeed. That’s why professional support makes all the difference. People who use structured programs-like counseling, nicotine patches, or medications like varenicline-are twice as likely to quit for good compared to those who try alone. In fact, 68% of patients who got help from their doctor quit successfully. Only 22% quit without support.
Medications: What Helps and What Doesn’t
There’s no cure, but medications can help you breathe easier and avoid flare-ups.- Bronchodilators (like albuterol or tiotropium) relax your airways. Short-acting ones work fast-within 15 minutes-for sudden breathlessness. Long-acting ones are used daily to keep things open.
- Inhaled steroids reduce inflammation, but they come with risks: higher chances of bone thinning, high blood pressure, and diabetes if used long-term.
- Mucolytics (like N-acetylcysteine) thin the mucus so it’s easier to cough up. Some guidelines say they’re useful; others don’t. But for people with thick, sticky mucus, they can make a real difference.
- Antibiotics are only for bacterial infections, not every cough. If you get a bad flare-up with yellow or green mucus and fever, your doctor might prescribe them.
Pulmonary Rehabilitation: The Hidden Game-Changer
If you’ve never heard of pulmonary rehab, you’re not alone. But it’s one of the most effective tools you have. Pulmonary rehab isn’t just exercise. It’s a full program: breathing techniques, nutrition advice, education on your condition, and supervised physical activity. People who complete it walk 78 meters farther in six minutes on average-and hospital visits drop by 37%. One study found that 78% of patients felt much better after rehab. They could do chores, play with grandkids, or take walks without gasping. And the best part? It’s covered by Medicare and most insurance plans. Doctors like Dr. MeiLan Han from the University of Michigan say rehab should be offered to everyone with chronic bronchitis, no matter how mild or severe. It’s not optional-it’s essential.Vaccines and Oxygen: Preventing the Worst
Because your lungs are already damaged, infections hit harder. That’s why vaccines matter:- Flu shot every year cuts your risk of a bad flare-up by 42%.
- Pneumococcal vaccine every 5-7 years protects against pneumonia, a common and dangerous complication.
Real Challenges: Why People Struggle
Knowing what to do is one thing. Doing it day after day is another. Many patients say:- Managing multiple inhalers is confusing.
- Side effects from steroids scared them into stopping.
- Exercise programs felt too hard, so they gave up after a few weeks.
- They didn’t realize how much quitting smoking would help-until it was too late.
What’s New in Treatment?
The field is moving forward. In 2023, the FDA approved a new drug called ensifentrine-a first-of-its-kind inhaler that helps open airways and reduce mucus. Early results show fewer flare-ups and better walking ability. Researchers are also studying gene variants that affect mucus thickness. Soon, doctors might be able to match you with the right mucolytic based on your biology. And digital tools are rising: inhalers with sensors that track when you use them, apps that guide breathing exercises, and virtual rehab sessions are making it easier to stick with treatment-even from home.What You Can Do Today
You don’t need to wait for the next big breakthrough. Start now:- If you smoke, call your doctor about a quit program. Don’t try alone.
- Ask for a spirometry test if you haven’t had one.
- Get your flu and pneumonia vaccines if you’re not up to date.
- Ask about pulmonary rehab. It’s not just for the very ill.
- Learn how to use your inhaler correctly. Ask for a demonstration.
- Track your symptoms: when you cough, how much mucus, when you get winded.
Final Thought: It’s Not About Perfection
You don’t have to quit smoking overnight. You don’t have to do rehab perfectly. You just have to start-and keep going. Chronic bronchitis doesn’t have to mean giving up your life. It means learning how to live better with it. And with the right support, that’s absolutely possible.Is chronic bronchitis the same as COPD?
Chronic bronchitis is one type of COPD, along with emphysema. COPD is the umbrella term for lung diseases that cause airflow blockage. If you have a long-term cough with mucus and breathing problems, you likely have COPD, and chronic bronchitis is probably the main part of it.
Can you get chronic bronchitis if you never smoked?
Yes, but it’s less common. About 10% of cases occur in people who never smoked. Causes include long-term exposure to air pollution, dust, fumes at work, secondhand smoke, or a rare genetic condition called alpha-1 antitrypsin deficiency. Still, smoking remains the leading cause by far.
How long does it take to see improvement after quitting smoking?
Within weeks, your lungs start to heal. Coughing and mucus production often decrease in 1-3 months. Breathing gets easier over 6-12 months. But the biggest benefit is long-term: quitting stops the disease from getting worse. People who quit after diagnosis slow lung decline by 60% compared to those who keep smoking.
Do I need oxygen therapy for chronic bronchitis?
Only if your blood oxygen levels are consistently low, usually below 88%. Your doctor will check this with a simple test. Oxygen therapy isn’t for everyone, but for those who need it, using it 15+ hours a day can extend life by years. It’s not a sign of being "terminal”-it’s a tool to help you live better.
Are inhalers the only treatment I need?
No. Inhalers help with symptoms, but they don’t fix the root cause. The most effective approach combines quitting smoking, pulmonary rehab, vaccines, and proper medication use. Many people rely only on inhalers and miss out on life-changing benefits like improved strength, fewer hospital visits, and better energy.


Adewumi Gbotemi
Man, I never thought about how much mucus is just your lungs screaming for help. My uncle smoked for 40 years and thought it was normal. He didn’t quit till he couldn’t walk to the bathroom without stopping. Now he walks every morning. Best thing he ever did.
Matthew Miller
Let’s be real - 90% of these cases are just people who refused to quit smoking and now want a medical excuse to feel sorry for themselves. Quitting isn’t hard. It’s just uncomfortable. And if you can’t handle discomfort, don’t blame your lungs. Blame your willpower.
Sam Davies
Oh wow, another ‘quit smoking or die’ manifesto. How original. I’m sure the 10% of non-smokers with chronic bronchitis are just thrilled to be lumped in with the ‘lazy smokers’ demographic. Next up: blaming climate change for your asthma? Maybe your cilia just had a bad day.
Also, ‘pulmonary rehab’ sounds like a spa day for people who forgot how to breathe. But sure, let’s make it sound like a miracle cure while ignoring the fact that most people can’t even afford the gas to get there.
Priscilla Kraft
This is so important 🙏 I had a patient last week who didn’t know her inhaler was supposed to be shaken. She’d been using it wrong for 5 years. A 5-minute demo changed her life. Please, if you’re on meds - ask for a demo. No shame. We’ve all messed up.
Jason Shriner
They say quitting smoking slows progression by 60%... but what if you’re already 70? What if your lungs are a graveyard? What if the real tragedy isn’t the cough... but the fact that no one told you this before you turned 50?
I’m not mad. I’m just... disappointed. In the system. In the doctors. In the fact that we wait until we’re gasping to care.
Sean Feng
Spit happens. Quit smoking. Done. Stop overcomplicating it with rehab and sensors and apps. If you can’t quit, you’re not sick - you’re addicted. And addiction isn’t a medical condition. It’s a choice. With consequences.
Jennifer Littler
The data on mucolytics is all over the place, but I’ve seen patients on NAC who went from coughing up tar balls to barely clearing their throat. It’s not magic, but it’s not placebo either. If you’ve got thick secretions, it’s worth a shot - especially if you’re not on steroids.
Alfred Schmidt
Why is it always about smoking?! What about the factory workers? The people breathing in diesel fumes in the city? The ones with alpha-1 deficiency who never touched a cigarette? You act like we’re all just lazy smokers who didn’t try hard enough. That’s not just reductive - it’s cruel.
And don’t even get me started on the oxygen tanks. I saw a woman cry because her neighbor called her ‘the oxygen lady.’ Like it’s a punishment. Like she chose this.
Vincent Clarizio
Let me break this down for you like you’re five: Your lungs are like a garden. Smoking is like dumping acid on the soil. The cilia are the worms. They’re supposed to turn the dirt, keep things clean. But acid kills the worms. Now the dirt is compacted. Mucus piles up. Fungi grow. You start coughing. You think it’s just a cold. It’s not. It’s a dying garden. And no inhaler is gonna fix acid in the soil. Only stopping the dumping will. And yes - it’s hard. But your garden is still alive. It’s not too late. You just have to stop pouring the acid.
Rehab is like hiring a gardener to teach you how to plant again. Vaccines are like fencing out the deer. Oxygen? That’s the sprinkler system when the drought hits. You don’t need all of it at once. But you need some. And you need to stop blaming the garden for being damaged.
I’ve seen people 80 years old start rehab. They walk 10 feet. Then 20. Then to the mailbox. Then to the bus stop. That’s not a miracle. That’s science. And dignity. Don’t let anyone tell you it’s too late. It’s never too late to stop pouring the acid.
And if you think this is just about quitting smoking - you’re missing the point. It’s about learning to live with what’s left. Not mourning what’s gone. And that’s the real work.
So stop scrolling. Stop comparing. Start breathing. One breath at a time.
Alex Smith
Interesting how the article says ‘not every smoker gets it’ - but then spends 90% of the time blaming smokers. So what’s the real variable? Genetics? Environment? Luck? Or just the fact that medicine loves a villain?
Also, why is ‘pulmonary rehab’ only for people who ‘have it bad’? Why isn’t it offered to every smoker over 40 as a preventive thing? Like a flu shot for your lungs? Hmm.
Christian Basel
Ensifentrine? Sounds like a drug designed by a marketing team that binge-watched sci-fi. Let me guess - $12,000 a year, covered by exactly zero insurers, and only available in ZIP codes with a Starbucks on every corner. Meanwhile, the guy in rural Ohio still can’t get his tiotropium refilled because his pharmacy doesn’t stock it. Cool. Real progress.
Priscilla Kraft
Just read the comment above - and I want to say: I’ve seen that exact thing happen. Rural clinics don’t stock newer meds. Patients get stuck with older ones that don’t work as well. It’s not about willpower. It’s about access. If you’re lucky enough to live near a hospital with a pulmonary program - you’re already ahead. Most aren’t. So yes - new drugs are cool. But let’s fix the basics first.