What Is CRPS, and Why Does It Hurt So Much?
Complex Regional Pain Syndrome, or CRPS, isn’t just a bad injury that won’t heal. It’s your nervous system getting stuck in a loop of fear and pain-even when the original wound is long gone. Imagine touching a cotton ball and feeling like your hand is on fire. Or trying to put on a sock and your brain screams danger, even though there’s no damage left. That’s CRPS. It often starts after a fracture, surgery, or sprain, but the pain doesn’t fade with the injury. Instead, it grows, spreading, intensifying, and rewiring how your brain reads touch, movement, and temperature.
Research shows about 26 in every 100,000 people get CRPS each year in the U.S., and most cases follow trauma. The pain isn’t just physical-it’s neurological. Your spinal cord and brain start misfiring. Areas that once controlled your hand or foot become confused, with neighboring brain regions taking over. This is called cortical smudging. Your body isn’t broken-it’s misinterpreting signals. That’s why painkillers often fail. You don’t need more drugs. You need to retrain your brain.
Desensitization: Rewiring Your Skin’s Alarm System
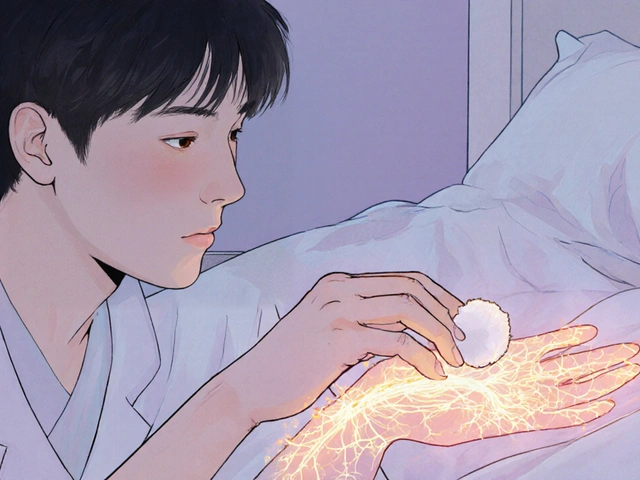
One of the most common symptoms of CRPS is allodynia-pain from something that shouldn’t hurt. A light brush of fabric, a breeze, even a bedsheet can feel like needles. Desensitization therapy isn’t about toughening up. It’s about teaching your nervous system that these sensations are safe.
The process starts slow. You begin with something softer than a feather-cotton balls, silk scarves, or even a soft makeup brush. Apply it for just 5 minutes at a time, 3 to 5 times a day. The pressure? Less than 10 grams-about the weight of a paperclip. You don’t push through pain. You stay under a pain level of 3 out of 10. If it spikes, you stop. You wait. You try again tomorrow.
Over 4 to 12 weeks, you slowly move to slightly rougher textures: felt, then terry cloth, then denim. Eventually, you reintroduce normal clothing. The goal isn’t to tolerate pain. It’s to prove to your brain that touch isn’t a threat. Studies using fMRI show this reduces overactive signals in the somatosensory cortex by 30-40% after just 8 weeks. One 2021 trial found patients using structured desensitization improved 42% more on hand function tests than those doing only stretching.
There are four clear phases:
- Phase 1 (Weeks 0-2): Passive touch with eyes open. You let someone else apply the stimulus while you watch.
- Phase 2 (Weeks 2-4): You start moving your fingers or toes while being touched. Movement helps reconnect brain pathways.
- Phase 3 (Weeks 4-8): You introduce temperature-cooling with a damp cloth, then warming with a warm towel.
- Phase 4 (Week 8+): You wear normal clothes, wash your hands, hold a coffee cup-all without panic.
Adherence is high-nearly 8 out of 10 patients stick with it. But it takes patience. On average, it takes 47 days to go from cotton to normal socks. The payoff? People report being able to hug their kids, sleep without pain, and finally wear shoes again.
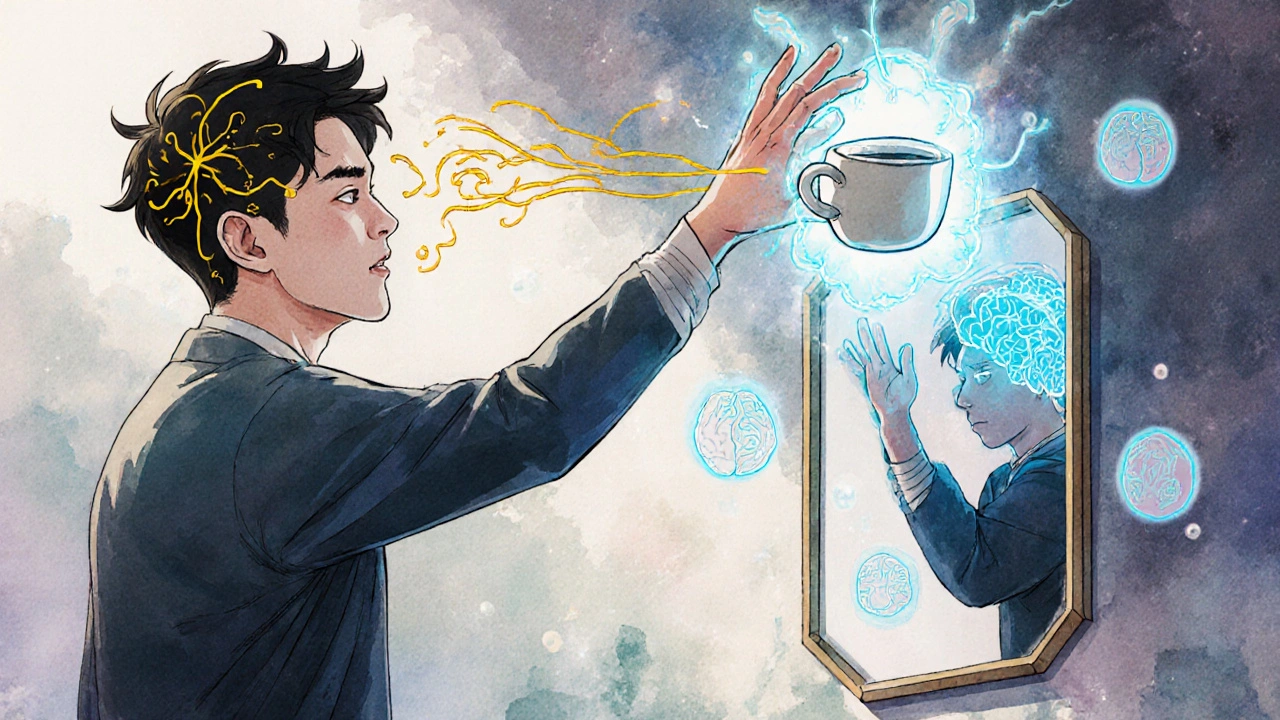
Graded Motor Imagery: Training Your Brain to Move Without Fear
While desensitization works on touch, Graded Motor Imagery (GMI) tackles movement. In CRPS, your brain forgets how to move the affected limb. Not because the muscles are weak-but because your brain thinks moving it will cause more pain. So it avoids it. And avoidance makes the problem worse.
GMI, developed by Dr. G. Lorimer Moseley, is a three-step method designed to reverse this brain confusion. It doesn’t require pain. It doesn’t require movement-at first.
Stage 1: Left/Right Discrimination
You look at pictures of hands or feet-some left, some right-and you identify them as fast as you can. No moving. Just deciding. You use flashcards or apps like Recognise Online. Start with 50 images a day. Aim for 90% accuracy in under 1.5 seconds per image. If you’re wrong, you don’t push. You rest. This stage trains your brain to recognize the limb as part of your body again. In CRPS, the brain’s map of the limb gets blurry. This sharpens it.
Stage 2: Explicit Motor Imagery
Now you imagine moving the limb-without moving it. Picture yourself picking up a cup, turning a doorknob, or typing. Do this for 5-10 minutes a day. Focus on the sensation of movement, not the pain. You’re not pretending it’s easy. You’re reminding your brain that movement doesn’t equal danger. Studies show this alone can reduce pain by 30% in just 2 weeks.
Stage 3: Mirror Therapy
Place a mirror vertically beside your affected limb. Cover the bad side. Move your healthy hand in front of the mirror. Your brain sees the reflection and thinks it’s the injured one moving. This tricks your brain into believing the painful limb is moving safely. Start with 5 minutes a day. Build to 20-30 minutes. Many patients report their limb warming up, swelling going down, and pain dropping within weeks.
A 2006 study by Moseley found 70% of CRPS patients had over 50% pain reduction after just 4 weeks of GMI. fMRI scans showed their brain’s motor and sensory maps returned to normal size. Another study found tactile discrimination improved-from being able to feel two points 15mm apart to just 7mm-meaning your skin’s sensitivity was returning to normal.
Why GMI Works Better Than Traditional Therapy
Traditional physical therapy for CRPS often focuses on stretching and strengthening. But if your brain is screaming danger, forcing movement can backfire. It reinforces fear. GMI doesn’t force. It reprograms.
A 2023 review of 33 clinical trials found GMI reduced pain by 2.8 points more on a 10-point scale than standard therapy. That’s not a small difference-it’s life-changing. People went from being unable to wash their hair to cooking meals again. Mirror therapy alone improved upper limb function 40% more than conventional rehab in post-surgery CRPS patients.
But GMI isn’t magic. It’s hard. The first two weeks often feel worse. Pain spikes. Frustration builds. One Reddit user said, “The first two weeks were brutal-I thought I was making it worse.” But by week six, they picked up a coffee cup for the first time in 18 months.
That’s why success depends on pacing. Push too fast, and you risk worsening symptoms. One study found 15% of patients got worse when therapists advanced GMI too quickly. That’s why training matters. Only therapists with at least 40 hours of specialized CRPS training should guide this. The American Physical Therapy Association says improper GMI accounts for 22% of treatment failures.
Putting It All Together: The Best Outcomes Come from Combining Methods
Desensitization and GMI work best together. One targets touch. The other targets movement. Both rewire the brain. But the strongest results come when you add one more piece: psychological support.
CRPS isn’t “all in your head.” But your head plays a huge role. Fear, anxiety, and trauma can lock the pain in place. Cognitive Behavioral Therapy (CBT) helps patients reframe thoughts like “I’ll never move again” into “I’m retraining my brain.”
Studies show the most successful programs combine all three: desensitization, GMI, and CBT. In one 2022 trial, patients using this trio saw a 5.2-point drop in pain on the 10-point scale after 24 weeks. That’s more than half the pain gone.
Timing matters too. If you start within 3 months of symptom onset, your chances of recovery jump to 83%. After 12 months? Only 42%. The sooner you begin, the better your brain can heal.
What to Expect-and What to Avoid
There’s no quick fix. GMI and desensitization take weeks, sometimes months. But the results are real. People report:
- Temperature returning to normal in the affected limb
- Swelling reducing without medication
- Being able to wear gloves, shoes, or jewelry again
- Sleeping through the night
- Returning to work or hobbies
But here’s what doesn’t work:
- Pushing through pain
- Skipping stages
- Doing it alone without guidance
- Waiting too long to start
Don’t try this on your own. Find a therapist trained in CRPS rehabilitation-ideally one certified by the Hand Therapy Certification Commission (HTCC) or trained in the NOI Group’s GMI program. If you’re in the UK, the NHS now mandates access to GMI within 4 weeks of referral. Ask your GP. Push for it.
What’s Next for CRPS Treatment?
The future is digital. Apps like Miro Therapeutics, cleared by the FDA, now guide patients through GMI with AI-driven progress tracking. A 2023 study found patients using these apps were 35% more likely to stick with treatment than those using paper flashcards. Telehealth is helping too-especially in rural areas where trained therapists are scarce. One study showed telehealth was 67% effective at delivering GMI remotely.
Research is expanding. The International Association for the Study of Pain has committed $15 million a year to CRPS rehab research through 2030. New studies are exploring how combining GMI with virtual reality and biofeedback could speed recovery even more.
But the core hasn’t changed. CRPS isn’t a muscle problem. It’s a brain problem. And the brain can heal-if you give it the right signals.

Ryan Anderson
This is hands-down the most clear, science-backed breakdown of CRPS rehab I’ve ever read. 🙌 Desensitization felt like magic when I started-cotton balls to socks in 6 weeks? Yes please. My hand stopped screaming at me.
PS: If you’re reading this and scared to try… just start with a feather. Seriously. You’ve got this.
Eleanora Keene
I can't tell you how many people I've sent this to. My sister had CRPS after a wrist fracture and she went from crying every time she touched a doorknob to holding her newborn last month. It wasn't easy, but this exact method? It worked. Thank you for writing this with such care.
Joe Goodrow
This is why America still leads in medical innovation. Other countries are still stuck on pills and surgery. We actually retrain the brain? That’s next-level. I hope the VA starts covering this. Our vets need this more than opioids.
Don Ablett
The neuroplasticity evidence presented here is compelling, particularly the fMRI data indicating cortical reorganization following structured desensitization protocols. One might reasonably infer that the somatosensory homunculus undergoes functional recalibration under consistent, low-threshold sensory input. The temporal progression outlined is methodologically sound.
Kevin Wagner
Y’ALL. I was in a wheelchair for 14 months because my foot felt like it was stuffed in a vise made of broken glass. I tried EVERYTHING. Physical therapy? Nah. Nerve blocks? Nope. Then I found GMI. First two weeks? I wanted to quit. Day 47? I put on my damn sneakers. Now I hike. I dance. I hug my dog without flinching. This isn’t therapy-it’s liberation. If you’re reading this and still doubting? Just start the damn cotton ball thing. Your future self will thank you.
gent wood
I've been practicing GMI for 11 weeks now, and I can confirm the mirror therapy component is transformative. The brain's ability to rewire itself through visual feedback is nothing short of extraordinary. I've noticed a marked reduction in autonomic symptoms-swelling, discoloration-and my hand temperature has normalized. This is not anecdotal. This is neurology.
Dilip Patel
Lmao all this fancy talk and you still need a therapist? In India we just use turmeric paste and prayer. Why waste money on mirrors and cotton balls? You people overthink everything. My cousin had CRPS and he just walked through the pain. Now he runs marathons. Stop overmedicalizing everything.
Jane Johnson
I find it concerning that this article implies patients can self-administer GMI. The literature clearly states that improper implementation exacerbates symptoms. Without professional oversight, this could be dangerous. Why is this being presented as a DIY solution?
Sean Hwang
I had CRPS after a bike crash. Tried all the meds. Nothing. Then my PT showed me the cotton ball thing. First day? Felt like a knife. Day 10? I could touch my jeans. Now I wear socks. No big deal. But it was a big deal to me. Just start slow. Don’t rush. You don’t need to be a hero.
Barry Sanders
So you're telling me we're paying thousands for therapists to wave mirrors around? This is why healthcare is broken. All this ‘brain retraining’ is just placebo with a fancy name. I bet 80% of these people would’ve recovered on their own.
Chris Ashley
bro i tried the mirror thing and i cried for 2 hours because it felt like my arm was moving but it wasn’t. then i stopped. i don’t think my brain can handle this.
kshitij pandey
In India, we have a tradition called ‘sahyog’-support through presence. My friend with CRPS had her family sit with her while she did GMI every day. No pressure. Just presence. She started holding her teacup again after 10 weeks. This method works, but love matters too. Don’t forget that.
Brittany C
The neuroanatomical reorganization observed in fMRI studies following GMI aligns with predictive coding models of pain perception. The reduction in cortical smudging suggests a normalization of somatotopic representation in the primary somatosensory cortex. This is a paradigm shift from nociceptive to neuromatrix-based intervention.
Sean Evans
This is why I hate ‘wellness’ culture. You spend 6 months doing cotton balls and mirror tricks instead of just getting a spinal cord stimulator like a normal person? You’re glorifying suffering. Painkillers aren’t evil-they’re tools. This feels like a cult. 🤡
Anjan Patel
I’ve been doing this for 18 months. I started with a feather. Now I play guitar. My wife says I’ve changed. Not because I’m pain-free-I’m not. But now I don’t hate my body. That’s the real win. Don’t chase the zero pain. Chase the peace.