When treating depression or Parkinson’s disease, Emsam (Selegiline patch) is a transdermal delivery system that releases the MAO‑B inhibitor selegiline through the skin over several days. It promises steadier blood levels and fewer dietary restrictions than oral MAO‑B blockers, but is it truly the best choice? This guide breaks down the science, the side‑effect profile, the price tag, and the most common alternatives so you can decide if the patch fits your needs.
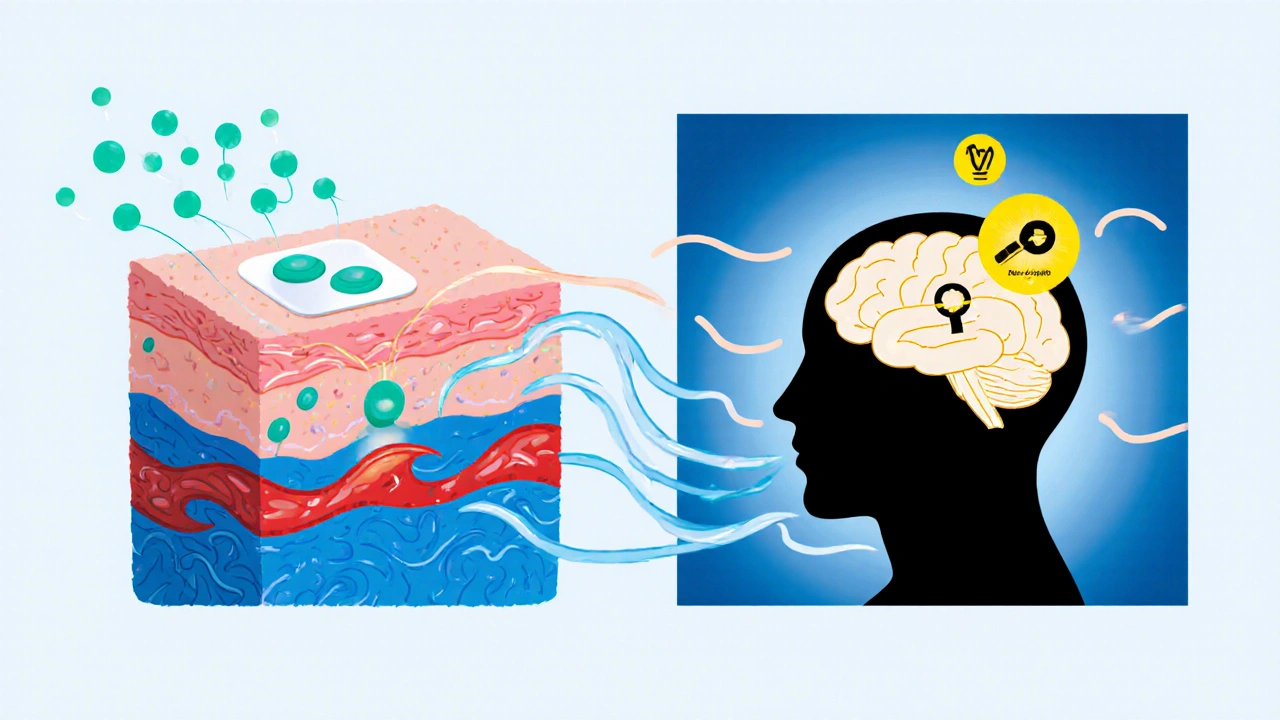
How the Emsam Patch Works
The patch contains 6 mg of selegiline, a selective irreversible inhibitor of monoamine oxidase‑B (MAO‑B). By blocking MAO‑B, it prevents the breakdown of dopamine, phenylethylamine, and other trace amines, thereby increasing their availability in the brain. Because the transdermal route bypasses the gastrointestinal tract, plasma concentrations stay within a narrow therapeutic window, reducing the risk of the classic "cheese reaction" linked to dietary tyramine.
Dosage, Administration, and Practical Details
- Apply one patch to clean, dry, hairless skin on the back, upper chest, or abdomen.
- Leave it on for 24 hours, then replace with a fresh patch.
- Typical dosing starts at 6 mg/24 h; some clinicians increase to 9 mg/24 h for Parkinson’s patients who need extra dopaminergic boost.
- No routine dietary restrictions are required at the 6 mg dose, but higher doses re‑introduce the tyramine warning.
Efficacy Overview
Clinical trials in major depressive disorder (MDD) have shown that the 6 mg/24 h patch yields response rates of 45‑50 % and remission rates around 30 %, comparable to many first‑line SSRIs. In Parkinson’s disease, the patch improves motor scores (UPDRS) by an average of 3‑5 points, similar to oral selegiline 10 mg daily.
Side‑Effect Profile
Because the patch avoids first‑pass metabolism, common gastrointestinal complaints (nausea, abdominal cramps) are less frequent than with oral selegiline. The most reported adverse events are mild skin irritation, dizziness, and insomnia. Rarely, patients experience hypertensive crises if they inadvertently consume high‑tyramine foods while on a 9 mg dose.
Cost and Insurance Considerations
In the United Kingdom, the Emsam patch is priced at roughly £120 for a 30‑day supply, making it more expensive than generic oral MAO‑B tablets (≈£30). Private insurance often classifies it as a “specialty drug,” which can increase out‑of‑pocket costs. However, some NHS formularies approve it for patients who cannot tolerate oral options.
Major Alternatives to the Emsam Patch
Below are the most widely used alternatives, grouped by mechanism of action.
- Oral Selegiline - the same molecule taken in tablet form (5‑10 mg daily). It requires strict dietary tyramine limits at higher doses.
- Rasagiline - a newer irreversible MAO‑B inhibitor, usually 1 mg daily, marketed for Parkinson’s and off‑label for depression.
- Safinamide - a reversible MAO‑B inhibitor with additional glutamate‑modulating effects, available in 50 mg and 100 mg tablets.
- Selective serotonin reuptake inhibitors (SSRIs) - e.g., sertraline, fluoxetine, first‑line for MDD.
- Serotonin‑norepinephrine reuptake inhibitors (SNRIs) - e.g., venlafaxine, duloxetine, useful for patients with mixed anxiety‑depressive symptoms.
- Mirtazapine - an atypical antidepressant that works via noradrenergic and specific serotonergic pathways.
- Bupropion - a norepinephrine‑dopamine reuptake inhibitor (NDRI) often chosen to avoid sexual side‑effects of SSRIs.
Side‑by‑Side Comparison
| Feature | Emsam (Selegiline patch) | Oral Selegiline | Rasagiline | Safinamide | SSRIs | SNRIs |
|---|---|---|---|---|---|---|
| Formulation | Transdermal patch (6 mg/24 h) | Tablet (5‑10 mg daily) | Tablet (1 mg daily) | Tablet (50 mg/100 mg daily) | Tablet/capsule (varies) | Tablet/capsule (varies) |
| Primary indication | Depression & Parkinson’s | Parkinson’s (off‑label MDD) | Parkinson’s (off‑label MDD) | Parkinson’s (off‑label MDD) | Major depressive disorder | Major depressive disorder |
| Mechanism | Irreversible MAO‑B inhibition | Irreversible MAO‑B inhibition | Irreversible MAO‑B inhibition | Reversible MAO‑B inhibition + glutamate modulation | Selective serotonin reuptake inhibition | Serotonin‑norepinephrine reuptake inhibition |
| Dietary tyramine restriction | None at 6 mg; required at 9 mg | Required at >10 mg | None | None | None | None |
| Common side‑effects | Skin irritation, insomnia, dizziness | Nausea, orthostatic hypotension | Headache, nausea | Dizziness, hypertension | Sexual dysfunction, GI upset | Increased blood pressure, insomnia |
| Typical cost (UK) | ~£120/30 days | ~£30/30 days | ~£50/30 days | ~£70/30 days | ~£20‑£40/30 days | ~£25‑£45/30 days |
| Insurance friendliness | Specialty‑drug tier | Generic tier | Generic tier | Generic tier | Generic tier | Generic tier |
When the Patch Makes Sense
If you’ve tried oral MAO‑B inhibitors and suffered from stomach upset, or if you’re worried about strict diet rules, the 6 mg Emsam patch is a strong candidate. Its steady plasma level also helps patients who experience “peaks and valleys” with tablets, especially those who have fluctuating motor symptoms in Parkinson’s disease.
When to Consider Alternatives
Cost‑sensitive patients often pick oral selegiline or generic SSRIs. If you need a rapid onset of action, an SNRI such as venlafaxine may work faster than a patch that builds up over a few days. For those with skin sensitivities, a patch isn’t ideal, so switching to rasagiline or safinamide avoids the irritation issue.
Practical Decision‑Tree
- Is your primary goal depression, Parkinson’s, or both?
- Depression only → Look at SSRIs, SNRIs, or bupropion first.
- Parkinson’s with depressive symptoms → MAO‑B inhibitors (patch or oral) are preferred.
- Do you have a history of skin reactions?
- Yes → Avoid the patch; choose oral selegiline, rasagiline, or safinamide.
- No → Continue to step 3.
- Is cost a major barrier?
- Yes → Oral generic options (selegiline, SSRIs) are cheaper.
- No → Evaluate efficacy and side‑effect profile.
- Do you need to avoid dietary tyramine?
- Yes, at any dose → Choose Emsam vs alternatives with a 6 mg patch or any reversible MAO‑B inhibitor (rasagiline, safinamide).
- No, you can manage diet → Any MAO‑B option works.
Key Takeaways
- The Emsam patch offers steady drug delivery and minimal diet restrictions at the 6 mg dose.
- It is pricier and can cause skin irritation, so weigh cost against convenience.
- Oral selegiline is cheaper but needs strict tyramine limits at higher doses.
- Rasagiline and safinamide provide comparable efficacy with simpler dosing and no diet concerns.
- For pure depression without Parkinson’s, SSRIs, SNRIs, or atypical agents like bupropion often remain first‑line due to cost and tolerability.
Frequently Asked Questions
Can I switch from oral selegiline to the Emsam patch without a washout period?
Yes. Because both products contain the same active ingredient, clinicians usually transition directly, monitoring for any skin reaction or sudden blood‑pressure changes during the first week.
Is the patch safe for people over 65?
Studies in elderly Parkinson’s patients show similar efficacy and a slightly higher rate of mild dermatitis, so regular site rotation and dermatologist consultation are advised.
Do I still need to worry about the “cheese reaction” on a 6 mg patch?
At the standard 6 mg/24 h dose, systemic MAO‑A inhibition is negligible, so typical tyramine‑rich foods are safe. Only the 9 mg dose re‑introduces that risk.
How long does it take for the patch to reach steady‑state levels?
Steady‑state plasma concentrations are usually achieved after 3‑4 days of consistent daily application.
Can the patch be used together with an SSRI?
Co‑administration raises the risk of serotonin syndrome, especially at higher MAO‑B doses. Clinicians generally avoid combining them unless under strict supervision.

Poornima Ganesan
First off, the Emsam patch isn’t just a gimmick; its steady transdermal delivery sidesteps the first‑pass metabolism that trips up oral MAO‑B inhibitors, meaning you get more predictable plasma levels. That alone can make a huge difference for patients who have been bouncing between peaks and valleys on tablets. The 6 mg dose also breezes past the tyramine‑rich diet restrictions that give many people anxiety about cheese and wine, which is a legit quality‑of‑life win. In terms of efficacy, the response rates hover around 45‑50 % for depression, putting it neck‑and‑neck with many first‑line SSRIs while offering a different side‑effect profile. For Parkinson’s, the motor score improvement is comparable to oral selegiline, so you’re not losing anything by swapping the route. The downside is price – at roughly £120 a month in the UK, it’s a pricey specialty drug compared to generic tablets that sit near £30. Skin irritation is another trade‑off; while most people shrug it off, a subset gets noticeable dermatitis that can be a deal‑breaker. Cost aside, the patch’s convenience factor is solid – just slap it on and forget about daily pills, which is great for adherence. If you’re already on oral selegiline, you can transition without a washout, but keep an eye on the site for any rash. Compared to rasagiline or safinamide, the patch doesn’t bring the extra glutamate‑modulating benefits of safinamide, but it also avoids the headache and nausea that sometimes accompany those agents. When you stack the pros and cons, the patch makes sense for people who struggle with gastrointestinal upset from oral meds, want to dodge strict diet rules, and can shoulder the higher cost. Conversely, if you’re cost‑sensitive, have a history of skin reactions, or need a rapid onset, oral alternatives or even standard SSRIs might be smarter choices. Bottom line: the patch is a solid option, but it’s not a universal silver bullet – weigh your personal priorities before committing.
Emma Williams
Sounds like a good overview.
James Mali
Honestly, I’ve tried the patch and it felt like a slow drip of hope – not exactly a morning jolt. The skin irritation part can be a nuisance if you’re prone to allergies. Still, the lack of dietary restrictions at the low dose is nice if you enjoy cheese.
Tracy O'Keeffe
Well, the patch is just another corporate gimmick, masquerading as innovation while pumping up the pharma profits. Its "steady delivery" is just a marketing buzzword; real neurochemistry cares about receptor dynamics, not how you stick a silicone square on your torso. If you’re truly seeking therapeutic nuance, you should consider the pharmacokinetic profiles of reversible inhibitors like safinamide, which offer modulatory benefits beyond mere dopamine preservation. Moreover, the patch’s cost is a blatant exploitation of patients desperate for "new tech" solutions, ignoring the fact that generic oral options have been clinically validated for decades. The so‑called convenience is a superficial veneer that masks underlying side‑effects like dermatitis and insomniac episodes, which can cascade into worsening depression. In short, don’t be swayed by glossy brochures – dig into the mechanistic literature before you hand over your hard‑earned cash.
Joe Moore
Did you ever notice how the pharma companies hide the fact that the patch’s adhesive is laced with micro‑nanoparticles that can influence brain chemistry? They want us to think it’s just selegiline, but there’s a hidden agenda to control our thoughts. The real story is that the patch is part of a larger surveillance network embedded by big tech, feeding data back to the labs. Stay alert, don’t let them patch you into their system.
Ayla Stewart
I appreciate the perspective, but the evidence for nanotech in the adhesive is not established. The patch’s primary component remains selegiline.
Stephanie Zaragoza
When evaluating a therapeutic modality such as the transdermal selegiline system, one must attend closely to both the pharmacodynamic implications and the systemic economic considerations. The patch, delivering 6 mg per 24 hours, offers a pharmacokinetic profile characterized by reduced peaks and troughs, thereby minimizing the fluctuation‑induced side‑effects commonly observed with oral formulations. Furthermore, the elimination of dietary tyramine restrictions at the standard dose confers a tangible improvement in patient quality of life, especially for those who maintain a varied diet. Nevertheless, the cost differential-approximately £120 per month versus £30 for generic oral selegiline-represents a non‑trivial barrier that can impede access for economically disadvantaged populations. Clinicians should also be vigilant regarding dermatologic reactions; although typically mild, they may necessitate site rotation or alternative therapy. In contrast, agents such as rasagiline and safinamide circumvent both cost and cutaneous concerns while providing comparable efficacy, albeit through slightly divergent mechanisms-irreversible versus reversible MAO‑B inhibition, respectively. Ultimately, the decision matrix must integrate individual patient preferences, comorbid conditions, and financial constraints to ascertain the most appropriate therapeutic pathway.
Janet Morales
Whoa, hold up! All that polite talk about “integrating preferences” sounds like a corporate script. The real deal is that the patch is just a pricey status symbol for those who think they’re smarter than the rest of us. If you wanted to actually help people, you’d push cheaper generics, not this $120 “luxury” gel. It’s absurd to celebrate a drug delivery system that turns a simple pill into a fashion accessory. Let’s stop glorifying pharma hype and focus on real, accessible care.
Rajesh Singh
Listen up, folks: we have a moral responsibility to champion treatments that respect both the body and the wallet. The Emsam patch, while scientifically elegant, leans heavily on an economic privilege that sidelines many patients in low‑income brackets. It’s not merely a medical device; it’s an emblem of a system that rewards those who can afford the premium. If we truly care about equity, we must demand that health authorities negotiate better pricing or prioritize affordable oral alternatives that deliver comparable outcomes without the sticker shock. In short, let’s not let glossy science cover up the underlying injustice.
Albert Fernàndez Chacón
That’s a fair point. Balancing efficacy with affordability is key.