Ezetimibe LDL-C Reduction Calculator
This tool estimates the potential LDL-C reduction when adding Ezetimibe to existing statin therapy.
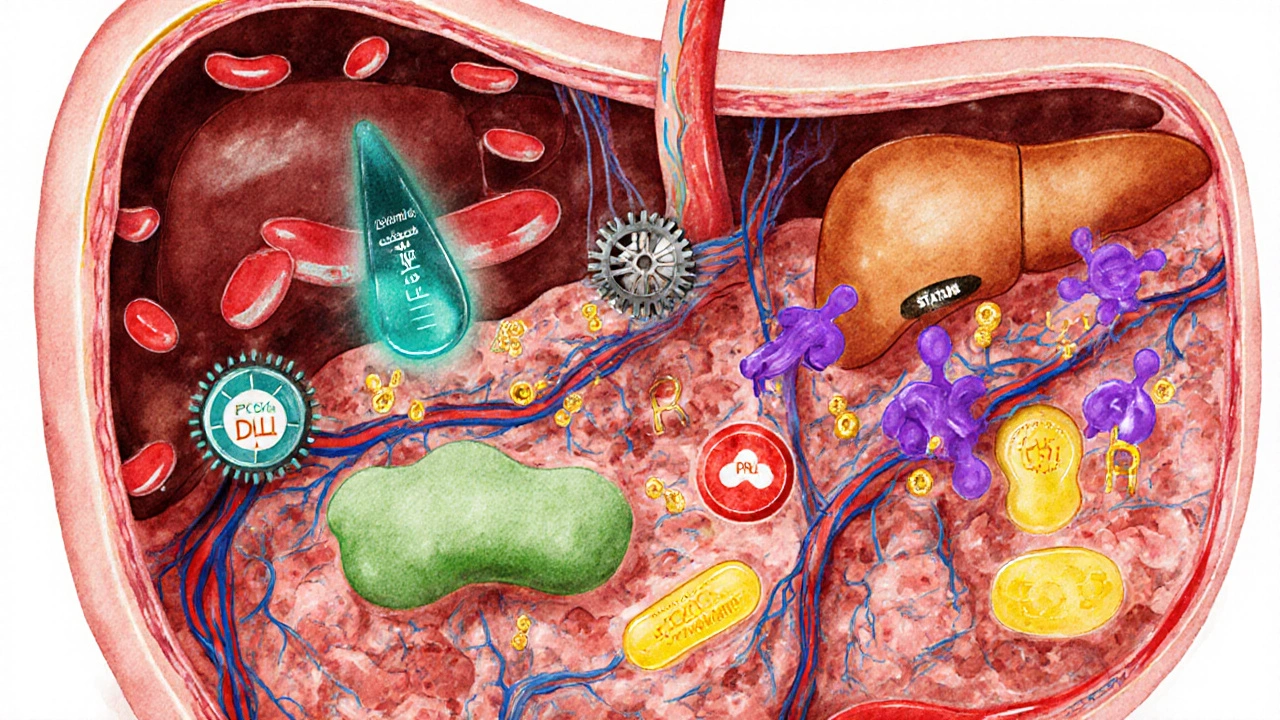
Did you know that high LDL‑C levels are responsible for over 4million deaths worldwide each year? Picking the right drug to clip those numbers can feel like a maze, especially when you hear names like statins, PCSK9 inhibitors, and bile‑acid binders tossed around. Below you’ll find a straight‑talk guide that walks you through how Ezetimibe stacks up against the most common alternatives, so you can decide what suits your health goals, budget, and lifestyle.
What is Ezetimibe?
Ezetimibe is a cholesterol‑lowering medication that blocks the absorption of dietary and biliary cholesterol in the small intestine. Approved in the UK in 2002, it’s often prescribed when statins alone don’t hit target LDL‑C levels or when patients can’t tolerate high‑dose statins.
How Ezetimibe Works
Unlike statins, which inhibit the liver enzyme HMG‑CoA reductase, Ezetimibe targets the NPC1L1 transporter on the brush‑border of intestinal cells. By reducing the amount of cholesterol that enters the bloodstream, it typically drops LDL‑C by 15‑20% as a solo therapy and up to 30% when paired with a moderate‑dose statin.
Key Alternatives to Consider
When the goal is to lower LDL‑C, the market offers several other classes. Below each drug class gets a quick rundown.
Statins (e.g., Atorvastatin)
Atorvastatin is a high‑intensity statin that reduces cholesterol synthesis in the liver. It remains the first‑line therapy in UK guidelines, delivering average LDL‑C reductions of 40‑55%.
PCSK9 Inhibitors (e.g., Evolocumab)
Evolocumab is a monoclonal antibody that blocks the PCSK9 protein, allowing more LDL receptors to clear cholesterol from the blood. Clinical trials show 55‑70% LDL‑C drops, but the price tag is steep.
Bile‑Acid Sequestrants (e.g., Cholestyramine)
Cholestyramine is a resin that binds bile acids in the gut, forcing the liver to use more cholesterol to make new bile acids. Expect a modest 10‑15% reduction, with gastrointestinal side effects being the most common complaint.
Fibrates (e.g., Gemfibrozil)
Gemfibrozil is a medication that activates PPAR‑α to increase the breakdown of triglyceride‑rich particles. While not a primary LDL‑C reducer, it shines for high triglycerides and can lower LDL‑C by 5‑10%.
Quick Comparison Table
| Drug/Class | Mechanism | Typical LDL‑C Reduction | Common Side Effects | UK Cost (per month) |
|---|---|---|---|---|
| Ezetimibe | Blocks intestinal NPC1L1 transporter | 15‑20% alone; 30% with statin | Headache, GI upset | £15‑£20 |
| Atorvastatin | Inhibits HMG‑CoA reductase | 40‑55% | Muscle pain, liver enzyme rise | £5‑£10 |
| Evolocumab | Blocks PCSK9 protein | 55‑70% | Injection site reaction, flu‑like symptoms | ~£600 (special funding) |
| Cholestyramine | Binds bile acids in gut | 10‑15% | Constipation, abdominal bloating | £8‑£12 |
| Gemfibrozil | Activates PPAR‑α | 5‑10% | GI upset, gallstones (rare) | £12‑£16 |
When Ezetimibe Is the Right Choice
Imagine a patient on a moderate dose of Atorvastatin who only reaches a 35% LDL‑C drop, still above the NHS target of 2.5mmol/L. Adding Ezetimibe can push the total reduction past 50% without upping the statin dose, sparing the patient from muscle‑pain risks. It’s also a go‑to for people with liver enzyme concerns, because it doesn’t tax the liver the way statins do.
Scenarios That Favor Other Options
- Statins only: For most primary‑prevention patients, a high‑intensity statin alone is enough and cheaper.
- PCSK9 inhibitors: Ideal for those with familial hypercholesterolemia or established cardiovascular disease who need a >50% drop and can access NHS specialist funding.
- Bile‑acid sequestrants: Useful when a patient cannot tolerate any systemic therapy and prefers a non‑absorbed agent.
- Fibrates: Best for patients whose main concern is high triglycerides rather than LDL‑C.
Decision Checklist for Clinicians and Patients
- Is the patient already on a maximally tolerated statin? If yes, consider Ezetimibe as an add‑on.
- Are liver enzymes elevated? Ezetimibe spares the liver; PCSK9 inhibitors are neutral too.
- What is the budget? Ezetimibe and generic statins are NHS‑friendly; PCSK9 inhibitors need approval.
- Any GI sensitivity? Bile‑acid sequestrants may aggravate it, while Ezetimibe usually causes mild upset only.
- Is the primary issue high triglycerides? A fibrate might be the better first step.
Practical Tips for Switching or Adding Therapy
Start by confirming the patient’s baseline LDL‑C and target level. If adding Ezetimibe, the usual dose is 10mg once daily, taken with or without food. Counsel patients that the drug may take 2‑4 weeks to show its full effect. For statin‑intolerant folks, a low‑dose statin + Ezetimibe combo often achieves goals with fewer muscle complaints.
Potential Pitfalls & How to Avoid Them
- Drug interactions: Ezetimibe is metabolized by CYP3A4; avoid strong inducers like rifampicin.
- Adherence: Because the benefit is modest, patients may stop early. Emphasize the additive effect when paired with statins.
- Insurance coverage: In the UK, most prescriptions are covered, but specialist‑only drugs need justification.
Bottom Line: Tailor the Choice to the Individual
There isn’t a one‑size‑fits‑all answer. If you need a cheap, well‑tolerated add‑on, Ezetimibe shines. If you require a dramatic LDL‑C plunge and can navigate specialist pathways, PCSK9 inhibitors win. Statins remain the backbone, while bile‑acid binders and fibrates fill niche gaps.
Frequently Asked Questions
Can I take Ezetimibe with a statin?
Yes. The most common regimen is a moderate‑intensity statin plus 10mg of Ezetimibe daily. This combo often achieves LDL‑C targets that either drug alone cannot reach.
What are the main side effects of Ezetimibe?
Most people tolerate it well. The typical complaints are mild headache and occasional gastrointestinal upset, which usually resolve on their own.
Is Ezetimibe suitable for people with liver disease?
Because it works in the intestine rather than the liver, Ezetimibe is considered safe for mild‑to‑moderate liver impairment. Always check liver function tests before starting any lipid‑lowering therapy.
How quickly will I see a drop in LDL‑C?
Ezetimibe can lower LDL‑C within 2weeks, but the maximum effect is usually evident after 4-6weeks. Repeat blood work at that point to gauge response.
Are there any foods I need to avoid while on Ezetimibe?
No specific dietary restrictions are required. However, maintaining a heart‑healthy diet supports the medication’s effect and overall cardiovascular risk reduction.


Brenda Taylor
Ezetimibe is cheap and works, why overcomplicate? :)
Dana Sellers
We need to remember that cholesterol isn’t just a number on a lab report; it’s a matter of staying healthy for our families. Taking cheap drugs like ezetimibe when they work is the responsible thing, not splurging on fancy options that most people can’t afford. It’s about doing the right thing for ourselves and for the community.
Damon Farnham
The pharmacodynamics of ezetimibe, when juxtaposed against the venerable statin class, reveal a nuanced interplay of intestinal absorption inhibition versus hepatic synthesis suppression, a distinction that is often obfuscated by lay discourse. One must appreciate, moreover, that the modest 15‑20% LDL‑C decrement attributable to monotherapy, while statistically insignificant to the neophyte, constitutes a clinically relevant bridge for patients intolerant to high‑intensity statins. Furthermore, the synergistic augmentation observed with concomitant statin administration-yielding up to a 30% reduction-underscores the therapeutic merit of a combinatorial regimen. It is incumbent upon the prescriber to scrutinize hepatic enzyme panels, for ezetimibe, unlike its hepatic‑centric counterparts, exerts minimal hepatic strain. Nevertheless, the specter of drug‑drug interactions via CYP3A4 metabolism, albeit modest, necessitates vigilant medication reconciliation. Economically, the drug’s price point, residing comfortably within the NHS formulary, offers a fiscally prudent alternative to the exorbitant PCSK9 inhibitors, whose cost often eclipses £600 per month. From a patient adherence perspective, the once‑daily 10 mg tablet, devoid of the gastrointestinal heft of bile‑acid sequestrants, fosters compliance. Clinical guidelines, while endorsing statins as first‑line therapy, have progressively elevated ezetimibe to a respectable second‑line status, particularly in the context of familial hypercholesterolemia. Critics, however, who deride the drug as a “me‑too” agent fail to acknowledge the mechanistic orthodoxy it introduces. Moreover, the evidence base, fortified by the IMPROVE‑IT trial, unequivocally demonstrates a marginal yet statistically significant reduction in cardiovascular events when ezetimibe is added to simvastatin. Adverse effects, predominantly mild headache and occasional gastrointestinal upset, are fleeting and seldom mandate discontinuation. In contrast, the muscular myopathy associated with high‑dose statins remains a palpable deterrent for many patients. Thus, the clinician, armed with an armamentarium of lipid‑lowering agents, must judiciously calibrate therapy to the individual’s risk profile, tolerability, and socioeconomic context. The decision matrix, albeit complex, can be distilled into a triad of efficacy, safety, and cost-domains wherein ezetimibe consistently demonstrates competence. In summation, to eschew ezetimibe solely on the grounds of modest efficacy would be a disservice to the nuanced art of personalized medicine.
Gary Tynes
hey damon i get what u say but i think ezetimibe is solid for folks who cant handle high statins it’s simple and low risk keep it up
Marsha Saminathan
Oh wow, diving into the world of cholesterol‑lowering meds feels like embarking on a vibrant safari across the savanna of biochemistry, where each drug is a dazzling creature with its own bold stripes and subtle spots. Ezetimibe, that tiny yet tenacious guardian of the gut, swoops in like a night‑owl, silently snatching cholesterol before it even dreams of slipping into the bloodstream. Meanwhile, statins march like disciplined soldiers, hammering the liver’s cholesterol‑making factories with relentless vigor. PCSK9 inhibitors, those glossy, high‑priced superheroes, burst onto the scene draped in fancy lab coats, promising dramatic drops that sound like miracles. Bile‑acid binders sit in the background, gritty and earthy, willing to sacrifice comfort for modest gains. Fibrates flutter about, bright as butterflies, chasing triglycerides with whimsical flair. The choice, dear reader, is a kaleidoscope of cost, side‑effects, and personal health narratives, each piece shimmering with potential. So strap on your explorer’s hat and let’s chart the best path together
Justin Park
Marsha, you’ve painted a vivid picture! I appreciate the colorful metaphor that makes the pharmacology feel alive 😊. From a mechanistic standpoint, ezetimibe’s inhibition of NPC1L1 is indeed a unique entry‑point compared to hepatic synthesis controls. It’s worth noting that while the dramatic reductions of PCSK9 inhibitors are impressive, the cost‑effectiveness analysis often tilts in favor of ezetimibe for average risk patients. Let’s keep the discussion grounded in both science and patient experience.
Herman Rochelle
Justin, great points. I agree that balancing efficacy and cost is key. Patients appreciate a clear plan that won’t break the bank.
Stanley Platt
In accordance with prevailing clinical guidelines, it is incumbent upon practitioners to evaluate lipid‑lowering strategies through a comprehensive lens that incorporates efficacy, safety, and economic considerations. Ezetimibe, as an adjunctive therapy, affords a modest yet statistically significant reduction in low‑density lipoprotein cholesterol, thereby occupying a strategic position within the therapeutic hierarchy. Moreover, its favorable tolerability profile and minimal hepatic impact render it a viable option for patients with statin‑associated myopathy. Nonetheless, clinicians must remain cognizant of the incremental benefit relative to the cost, particularly when juxtaposed against high‑intensity statins or novel agents such as PCSK9 inhibitors. Ultimately, individualized patient assessment remains the cornerstone of optimal lipid management.
Alice Settineri
Stanley, you’ve nailed the formal vibe, but let’s spice it up! Ezetimibe isn’t just a modest side‑kick; it’s the secret sauce that can turn a bland cholesterol plan into a fireworks show. Think of it as the underdog hero that punches above its weight, especially when budgets scream “no more pricey injections!” So, why not give it a standing ovation and let patients feel the power?
Dawson Turcott
Oh great, another cheap pill that “maybe” works 🙄
Alex Jhonson
Dawson, while your cynicism is noted, the evidence does suggest modest benefits, especially when combined with statins. Perhaps we could explore the data together?
Katheryn Cochrane
Let’s cut through the fluff: ezetimibe is just a stop‑gap for patients who can’t tolerate the real workhorses. Its ~20% LDL‑C drop is laughably underwhelming compared to the 50‑plus percent you get from proper statin titration or a PCSK9 blocker. The marketing hype masks the fact that it’s a gimmick for pharma’s profit margins. Side‑effects are rare, sure, but the drug’s limited efficacy makes it a waste of prescription slots. If a doctor resorts to ezetimibe first, it signals a lack of confidence in proven therapy. Bottom line: reserve it for truly statin‑intolerant cases, not as a blanket add‑on.
Michael Coakley
Ah, the cynic’s chorus rings loud, yet philosophy reminds us that “the journey of lowering LDL is as valuable as the destination.” Perhaps ezetimibe’s modest claim holds its own poetry in the grand tapestry of cardiovascular care.