Medication Fall Risk Assessment Tool
Every year, more than 36 million older adults in the U.S. fall. About one in four of them ends up in the emergency room. And for many, the root cause isn’t slippery floors or poor lighting-it’s the very medications they’re taking to feel better. Sedating drugs like benzodiazepines, antidepressants, opioids, and muscle relaxants quietly increase fall risk by slowing reaction time, causing dizziness, and fogging judgment. The good news? These falls aren’t inevitable. With the right approach, you can cut that risk significantly-even while keeping essential treatments.
What Makes a Medication a Fall Risk?
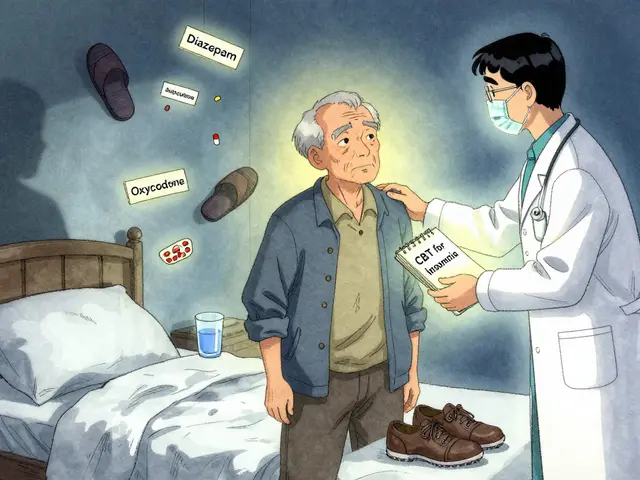
Not all meds are created equal when it comes to balance and safety. The ones that pose the highest danger are those that affect the central nervous system. These include:- Benzodiazepines (like diazepam or lorazepam) for anxiety or insomnia-these can cause next-day drowsiness and confusion.
- Antidepressants, especially tricyclics (amitriptyline) and SSRIs with sedating effects-studies show taking two or more increases fall risk by up to 70%.
- Opioids (oxycodone, hydrocodone)-even at low doses, they slow coordination and impair thinking.
- Muscle relaxants like baclofen-this one has the highest documented fall risk among its class.
- Antipsychotics (used for dementia-related behaviors)-they can cause orthostatic hypotension, making you dizzy when standing.
- Antihypertensives-if blood pressure drops too fast, it can trigger lightheadedness.
It’s not just the drug itself-it’s the combo. Taking three or more of these together? That’s polypharmacy, and it multiplies the danger. One study found that older adults on four or more sedating meds had nearly triple the fall risk compared to those on none.
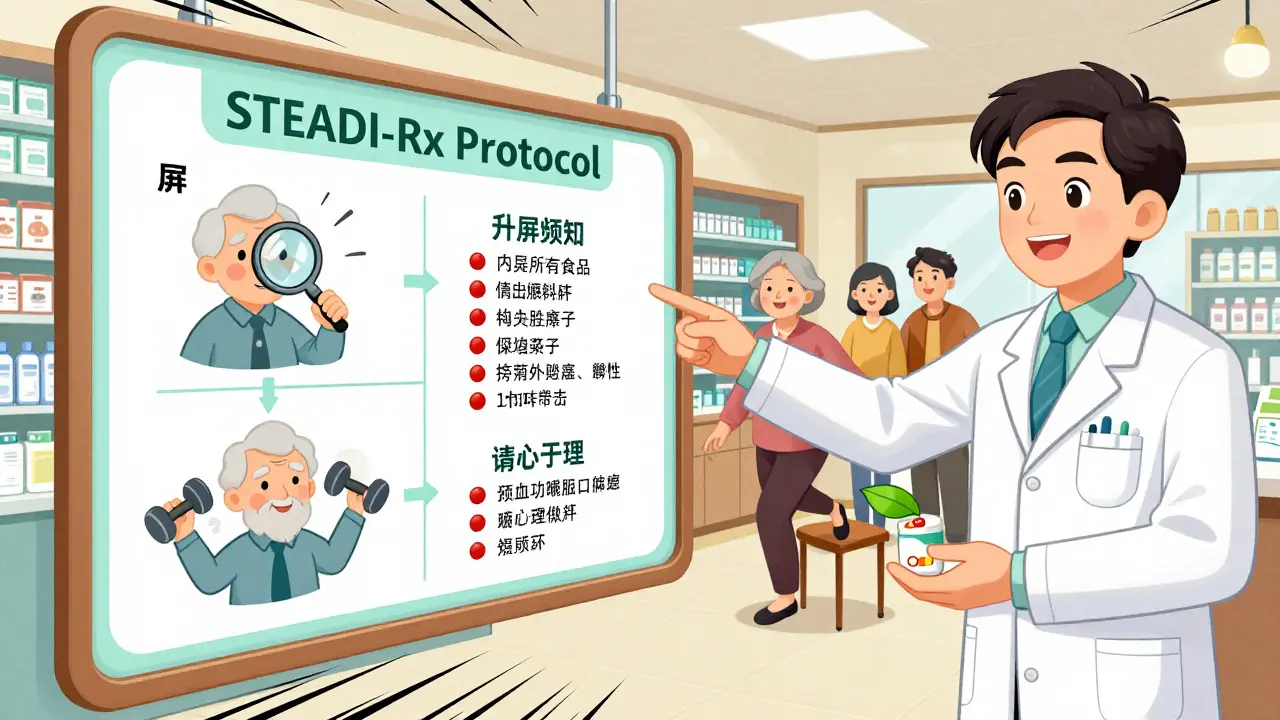
The STEADI-Rx Protocol: A Proven System
The CDC’s STEADI-Rx initiative isn’t just another guideline-it’s a working model that’s already helping thousands. Developed in partnership with the University of North Carolina and rolled out in community pharmacies since 2019, it’s built on three simple steps:- Screen-Ask if the person has fallen in the past year, feels unsteady, or fears falling. A simple yes to any means higher risk.
- Assess-Review every medication on the list. Pharmacists flag Fall Risk Increasing Drugs (FRIDs) using the Beers Criteria, a trusted reference updated every three years by the American Geriatrics Society.
- Intervene-This is where real change happens. Instead of just stopping meds, the goal is to swap them for safer alternatives.
Here’s what works: In the original STEADI-Rx study, 75% of pharmacist recommendations involved switching a sedating drug to a non-sedating one. For example, replacing diazepam with cognitive behavioral therapy for insomnia, or switching from amitriptyline to sertraline (a less sedating antidepressant). These swaps didn’t just reduce falls-they improved sleep, mood, and daily function.
Medication Review Isn’t Enough Alone
A 2022 Cochrane review showed that medication review alone reduces falls-but not nearly as much as when paired with exercise. The most effective strategy combines both. People who did balance training, strength work, and gait exercises three times a week for at least 12 weeks cut their number of falls by 15% to 29%. Those who also had their meds reviewed saw an even bigger drop.Why does exercise help so much? Because sedating drugs don’t just slow your brain-they weaken your body. Strength training rebuilds muscle. Balance drills retrain your inner ear and nervous system. You don’t need fancy equipment. Simple things like standing on one foot while brushing your teeth, heel-to-toe walking, or using a chair for support during leg lifts make a measurable difference.
And yes, vitamin D still comes up. The U.S. Preventive Services Task Force recommends 800 IU daily for older adults, but results are mixed. Some studies show benefit; others don’t. Still, if someone’s vitamin D level is low, supplementing is low-risk and may help bones stay strong if a fall does happen.
Real Stories, Real Results
On Reddit’s r/geriatrics forum, a user named u/SeniorSafetyFirst shared how switching from diazepam to CBT for insomnia cut their nighttime falls from 2-3 per month to zero over six months. Others reported similar wins after replacing sleep aids with melatonin or non-drug sleep hygiene. One man stopped taking a muscle relaxant after his pharmacist flagged it, and within weeks, he could walk his dog without holding onto walls.But it’s not always easy. A 2021 survey by the National Council on Aging found that 63% of older adults resisted cutting meds because they feared withdrawal symptoms or thought the drug was necessary. A woman on a benzodiazepine for anxiety told her doctor she couldn’t quit-it was her only way to sleep. Her pharmacist worked with her prescriber to taper slowly over 10 weeks, added daily walking, and introduced mindfulness techniques. After four months, she slept better than ever-and hadn’t fallen once.
Who Does What? The Team Approach
This isn’t a solo job. It takes a team:- Pharmacists are on the front lines. They review prescriptions, spot dangerous combinations, and talk to patients in plain language.
- Primary care doctors need to be open to deprescribing. Many still think stopping meds equals abandoning care-but it’s the opposite. It’s precision medicine.
- Physical therapists design safe, personalized exercise plans. They don’t just teach balance-they adapt it to your home, your pace, your fears.
- Family members can help track falls, note side effects, and support changes. A daughter who notices her dad stumbling after his new pain pill isn’t overstepping-she’s saving his life.
Communication is key. The STEADI-Rx model uses a Provider Consult Form so pharmacists can clearly share concerns and suggestions with prescribers within 7 days. If there’s no response, they follow up. That kind of structure makes a difference.

Barriers and How to Overcome Them
There are real obstacles. Many doctors don’t have time for full med reviews. Pharmacists report only 45% have enough time to do them well. Insurance doesn’t always pay for medication therapy management. Patients fear side effects from stopping meds. Prescribers worry about rebound anxiety or insomnia.Solutions exist:
- Electronic alerts in EHRs can flag high-risk meds before they’re prescribed.
- Standardized tools like the CDC’s fall risk checklist make reviews faster and more consistent.
- Reimbursement changes are slowly coming-Medicare now covers medication therapy management for certain patients.
- Education for patients: “This med helps your pain, but it also makes you dizzy. Let’s try a lower dose or something else.”
And don’t underestimate the power of small wins. If a patient agrees to cut one sedating pill and start walking 10 minutes a day, that’s progress. You don’t need to fix everything at once.
What’s Next? The Future of Fall Prevention
The field is evolving fast. In 2023, the CDC added new deprescribing guides for benzodiazepines and opioids. The American Society of Consultant Pharmacists now certifies Geriatric Pharmacotherapy Specialists-over 1,200 are already trained. AI tools are being tested to predict which medication combinations are most dangerous for individual patients. Some states are expanding pharmacists’ prescribing authority so they can switch meds directly, without waiting for a doctor’s approval.Demographics are pushing this forward. By 2040, nearly 81 million Americans will be over 65. Falls will keep rising unless we act. The cost? $50 billion a year in medical bills. But the bigger cost is loss of independence. Every fall avoided means someone keeps living at home, cooking their own meals, seeing their grandkids.
It’s not about taking away meds. It’s about choosing better ones. It’s about pairing safety with strength. It’s about listening to patients, trusting pharmacists, and moving together-meds, muscles, and mind.
Can sedating medications cause falls even if I haven’t fallen before?
Yes. Many people don’t fall until they’ve been on sedating meds for months or years. These drugs slowly erode balance, reaction time, and spatial awareness. You might not notice the changes until you trip on a rug or stumble getting out of bed. That’s why proactive review is so important-even if you’ve never fallen, if you’re on one or more of these drugs, your risk is higher than you think.
Is it safe to stop taking a sedating medication on my own?
No. Stopping certain sedating drugs suddenly-like benzodiazepines or antidepressants-can cause seizures, severe anxiety, rebound insomnia, or even delirium. Always work with your doctor or pharmacist to create a slow, safe tapering plan. They’ll monitor your symptoms and adjust the pace based on how you respond.
What’s the difference between STEADI and STEADI-Rx?
STEADI (Stopping Elderly Accidents, Deaths & Injuries) is the CDC’s overall fall prevention program, covering home safety, vision checks, and exercise. STEADI-Rx is the specific part focused on medications. It gives pharmacists and prescribers a step-by-step protocol to review, assess, and adjust drugs that increase fall risk. Think of STEADI-Rx as the medication arm of STEADI.
Can I still take pain medication if I’m at risk for falls?
Yes, but you need to be smarter about it. Opioids are high-risk. Non-opioid options like acetaminophen, topical NSAIDs, or physical therapy may be safer. If you need opioids, use the lowest effective dose for the shortest time possible. Combine it with balance exercises and avoid alcohol. Your pharmacist can help you weigh risks and explore alternatives.
How often should medication reviews happen for older adults?
At least once a year, but ideally every 6 months if you’re on three or more medications. If you’ve recently fallen, changed doctors, started a new drug, or noticed dizziness or confusion, get a review right away. Medications aren’t set in stone-they should be reviewed as often as your blood pressure or cholesterol.
If you or someone you care about is on sedating meds, don’t wait for a fall to happen. Talk to your pharmacist today. Ask: “Could any of my medications be making me unsteady?” That simple question could be the first step to staying safe, strong, and independent.

Coral Bosley
This is the kind of post that makes me want to cry and scream at the same time. My grandma was on five of these meds, and no one ever told her they were making her wobble like a newborn giraffe. She fell three times in six months, broke her hip, and spent the last year of her life in a wheelchair. All because doctors thought 'it's just a little drowsiness' and pharmacists were too busy counting pills to notice she couldn't stand up straight. We need to stop treating elders like walking pharmacy shelves.
MARILYN ONEILL
Wow. So you're saying we should just stop giving old people medicine? That's wild. Next you'll tell us to stop giving insulin to diabetics because it makes them sleepy. People need their meds. If they fall, it's because they're old, not because of drugs. Maybe they should just stop walking.
Steve Hesketh
Bro, I just want to say this hit me right in the soul. My dad is 78 and on three of these meds-he’s been walking with a cane since last year, but he still insists he’s fine. I showed him this article and he actually cried. We’re starting CBT for his insomnia next week. He’s scared, but he’s trying. You’re not alone. We’re all just trying to keep the people we love standing up. One step at a time.
shubham rathee
this is all a big pharma scam to sell more drugs and then sell you rehab and walkers and wheelchairs after you fall the drugs are not the problem its the hospitals and insurance companies making money off your fear and confusion the real enemy is the medical industrial complex and the government lets them do it because they get paid by the same people who make the drugs and the CDC is just a front for big pharma
MAHENDRA MEGHWAL
While the statistical evidence presented is compelling, one must consider the ethical implications of deprescribing in elderly populations. The autonomy of the individual, the potential for iatrogenic harm through abrupt discontinuation, and the psychological dependence on pharmacological reassurance must all be weighed with the utmost care. A systematic, multidisciplinary approach remains indispensable.
Sangeeta Isaac
so like… i’m 42 and my mom is on a muscle relaxant and she just told me last week she’s been holding onto the fridge to get to the sink. i thought she was just being dramatic. turns out she’s been falling every other night and didn’t tell anyone because she didn’t want to be a ‘burden.’ i’m taking her to the pharmacist tomorrow. also, i’m gonna start doing heel-to-toe walks while brushing my teeth. i’m not gonna wait until i’m 80 to figure this out.
Ben McKibbin
Let’s be real-this isn’t about meds. It’s about society’s refusal to accept that aging means decline. We want our grandparents to be spry and independent, but we won’t pay for home modifications, physical therapy, or pharmacist consults. We’d rather blame the drugs than fix the system. STEADI-Rx is great, but it’s a Band-Aid on a broken leg. We need universal geriatric care, not just pill-swapping.
Melanie Pearson
This is exactly why we can’t have nice things. The U.S. is falling apart because we treat the elderly like liabilities instead of citizens. If they can’t walk safely, they shouldn’t be allowed to live alone. These meds are prescribed because they’re necessary. Stop blaming doctors and start blaming the culture that lets people live in unsafe homes with no support. This isn’t a medical issue-it’s a moral failure.
Uju Megafu
OH MY GOD. My cousin’s husband took his own life last year because he was ‘depressed’ and on an SSRI. Everyone said it was ‘just depression.’ But he was dizzy, confused, and falling every day. No one checked his meds. No one asked if the drug was making him feel worse. He was 71. They didn’t even call it a fall. They called it ‘an accident.’ I’m done. This is murder by prescription.
Barbara Mahone
I’ve been a geriatric nurse for 32 years. I’ve seen this play out a thousand times. The quiet ones-the ones who don’t complain-are the ones who fall. They don’t want to be a burden. They don’t want to be told they’re too old. So they don’t say anything. Until they’re in the ER. This article? It’s not new. But it’s needed. Thank you for writing it.
Kelly McRainey Moore
my grandpa started walking his dog every morning after his pharmacist switched him from amitriptyline to sertraline. he said he felt like himself again. he even started baking again. i cried. this stuff works.
Ashok Sakra
why dont you just tell them to stop taking meds and go do yoga? its so easy right? everyone knows yoga fixes everything. also i saw a guy fall on tiktok and he was on no meds so its clearly just bad luck.
lokesh prasanth
meds are not the problem the problem is people dont respect their bodies anymore and think pills are magic. the real solution is discipline and fasting and sun exposure
Samuel Mendoza
So you’re saying the CDC knows better than 50 years of medical practice? That’s hilarious. Benzodiazepines have been used safely for decades. This is just another panic-driven trend. People fall because they’re old, not because they’re on lorazepam. Also, why are pharmacists making medical decisions? That’s not their job.