Heart disease isn’t just something that happens to older people. It can start quietly, years before symptoms show up. And the scary part? Most cases are preventable. The World Health Organization says heart disease kills nearly 18 million people every year-more than any other cause. But here’s the good news: about 80% of premature heart attacks and strokes can be avoided if you know your risks and act on them.
What You Can’t Change: Age, Sex, and Family History
Some risks are out of your hands. That doesn’t mean you’re doomed-it means you need to be smarter about the things you can control.Age is the biggest non-modifiable risk factor. After 45 for men and 55 for women, your risk starts climbing. By 70, about 70% of men and 60% of women will develop some form of heart disease. Each decade adds roughly 10% more risk, even if you eat right and exercise. Why? Arteries stiffen. Blood pressure creeps up. The heart muscle works harder. It’s not inevitable, but it’s common.
Men are more likely to have heart attacks earlier than women. But after menopause, women’s risk catches up-fast. That’s because estrogen, which helps protect blood vessels, drops sharply. So if you’re a woman over 60, don’t assume you’re safe just because you’re not a man.
Family history matters more than most people think. If a parent or sibling had heart disease before age 55 (for men) or 65 (for women), your risk jumps by 60% to 75%. It’s not just bad luck-it’s genetics. Some people inherit a tendency for high cholesterol, high blood pressure, or even a gene variant called 9p21 that increases risk by 20-30% per copy. Then there’s familial hypercholesterolemia, a genetic condition affecting 1 in 250 people. Left untreated, it can cause heart attacks in your 30s or 40s. If anyone in your family had a heart attack young, talk to your doctor. Get tested.
What You Can Change: The Big Four
The American Heart Association says if you fix just three things-smoking, high blood pressure, and inactivity-you could prevent nearly half of all heart deaths in the U.S. Here’s how they stack up.Smoking: The #1 Preventable Killer
Smoking doesn’t just hurt your lungs. It wrecks your arteries. Every cigarette damages the lining of your blood vessels, makes your blood stickier, and raises your blood pressure. Current smokers are 2 to 4 times more likely to have heart disease than non-smokers. Even smoking 1 to 5 cigarettes a day increases your risk by 50%, according to a 2020 JAMA study.The good news? Quitting works fast. Within one year, your risk drops by half. After 15 years, it’s almost the same as someone who never smoked. There’s no magic pill or patch that does this. But support programs, counseling, and medications like varenicline or nicotine replacement can double your chances of success.
High Blood Pressure: The Silent Saboteur
About 47% of U.S. adults have high blood pressure-and nearly half don’t know it. That’s why it’s called the silent killer. When your blood pressure stays above 130/80, your heart has to pump harder. Over time, this strains your heart, weakens arteries, and increases your chance of stroke or heart attack.Controlling it can cut your risk by 300-400%. The SPRINT trial showed that lowering systolic pressure to under 120 (instead of the old target of 140) reduced heart events by 25% in high-risk people. That means cutting salt, eating more potassium-rich foods (like bananas, spinach, sweet potatoes), moving daily, and taking medication if needed.
Cholesterol and Diabetes: The Hidden Duo
High LDL (“bad”) cholesterol clogs arteries. Nearly 94 million U.S. adults have levels too high. But it’s not just about the number-it’s about how long it’s been there. Years of high cholesterol silently build plaque. Statins can lower risk by 25-35% in those with existing heart disease.Diabetes is even scarier. If you have it, your risk of heart disease is 2 to 4 times higher. And 68% of people with diabetes over 65 die from heart problems. That’s not a coincidence. High blood sugar damages blood vessels and nerves that control your heart. Managing HbA1c below 7% helps-but newer diabetes drugs like SGLT2 inhibitors and GLP-1 agonists actually reduce heart attacks and death, even beyond lowering sugar.
Weight and Inactivity: The Quiet Contributors
Being overweight doesn’t directly cause heart disease-but it feeds the fire. It raises blood pressure, worsens cholesterol, and often leads to diabetes. Losing just 5-10% of your body weight can significantly lower all three.Physical inactivity is just as dangerous. People who sit all day have a 30-50% higher risk of heart disease than those who move regularly. You don’t need to run marathons. Walking 30 minutes a day, five days a week, cuts risk by 30%. Strength training twice a week helps too-it improves insulin sensitivity and lowers blood pressure.
When Risks Multiply: The Deadly Combo
The biggest danger isn’t having one risk factor. It’s having two or three together.Having both high blood pressure and diabetes? That raises your heart disease risk by 8 to 10 times compared to having neither. Smoking plus high cholesterol? That’s a one-two punch. Obesity plus inactivity? It’s like pouring gasoline on a fire.
Doctors call this synergy. It’s why simple checklists don’t work. If you have multiple risks, you need a plan-not just advice. That’s where tools like the ASCVD Risk Estimator come in. It uses your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking habits to calculate your 10-year risk. If it’s above 20%, you’re in the high-risk zone-and you need aggressive action.
What About Stress, Sleep, and Pollution?
These aren’t on the classic list-but they matter.Chronic stress raises cortisol, which increases blood pressure and inflammation. Poor sleep (under 6 hours a night) is linked to higher cholesterol, weight gain, and insulin resistance. And air pollution? A 2022 global study found that every 10 μg/m³ increase in PM2.5 (fine particle pollution) raises heart disease death risk by 10-15%.
It’s not just about your choices. Where you live, your job, your income-these social factors account for 30-50% of heart disease risk. People in low-income neighborhoods are 2-3 times more likely to die from heart disease. That’s not genetics. That’s access to healthy food, safe places to walk, clean air, and quality healthcare.
Your Action Plan: The ABCS Framework
The CDC’s Million Hearts initiative gives you a simple roadmap: ABCS.- Aspirin? Only if your doctor says so. Not for everyone.
- Blood pressure: Know your numbers. Aim for under 130/80.
- Cholesterol: Get tested. If you’re high risk, statins may be necessary.
- Stop smoking: No exceptions. Quitting is the single best thing you can do.
Start here:
- Get your blood pressure checked at least once a year.
- Ask for a cholesterol panel if you’re over 40-or earlier if you have family history.
- Take a walk every day. Even 10 minutes counts.
- If you smoke, call a quitline. Use apps like Smokefree or text-based programs. They work.
- Know your family history. Write it down. Share it with your doctor.

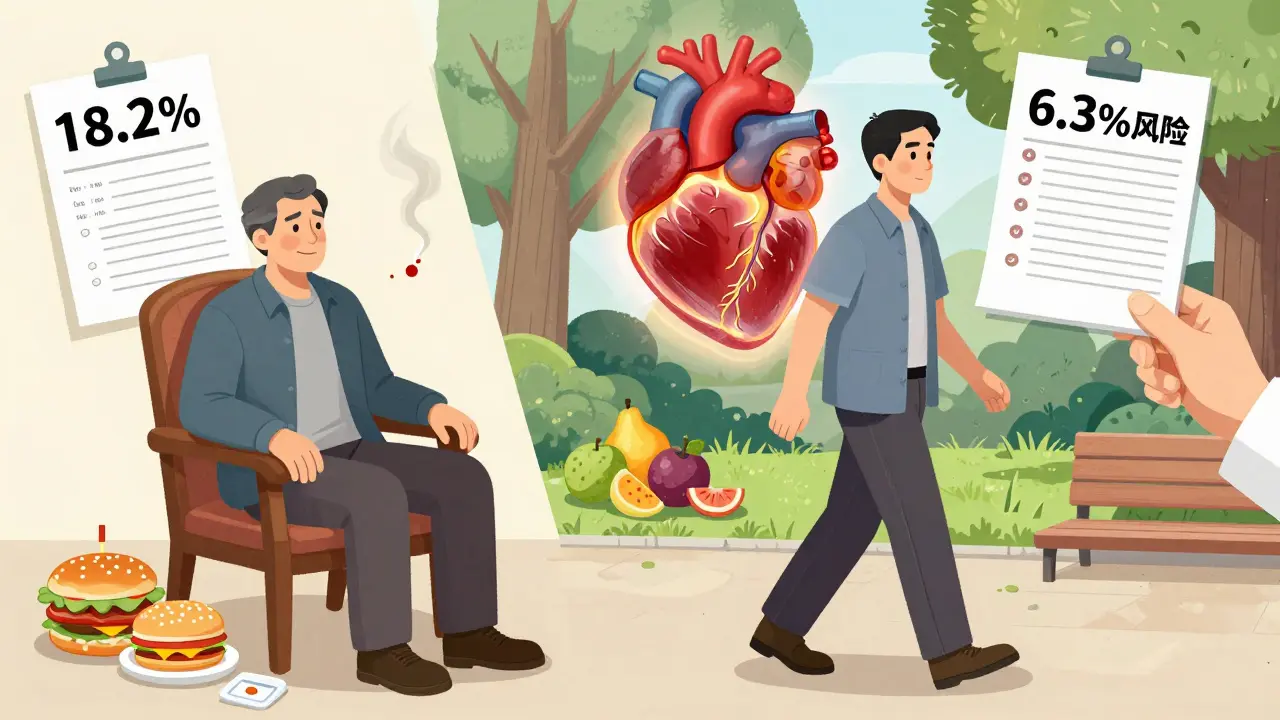
It’s Not About Perfection
You don’t need to be flawless. One man, 48, with smoking, obesity, high blood pressure, and family history lowered his 10-year heart attack risk from 18.2% to 6.3% in 18 months-not by going vegan or running 10Ks, but by quitting smoking, walking daily, and taking his meds. He didn’t have to be perfect. He just had to start.Heart disease isn’t a death sentence. It’s a warning sign. And the earlier you respond, the more power you have to change the outcome.
Can you have heart disease with no family history?
Yes. About 70% of people who have heart attacks don’t have a strong family history. Lifestyle factors like smoking, poor diet, inactivity, and high blood pressure are the main drivers for most cases. Family history increases your risk, but it doesn’t determine your fate.
Is heart disease only a problem for older adults?
No. While risk increases with age, plaque buildup starts in your 20s and 30s. Young adults with obesity, diabetes, or smoking habits are now having heart attacks in their 30s and 40s. The earlier you address risks, the better your long-term outcome.
Does quitting smoking really help if you’ve smoked for 30 years?
Absolutely. Even after decades of smoking, quitting cuts your heart disease risk in half within one year. After 15 years, your risk is nearly the same as someone who never smoked. Your arteries begin healing almost immediately after your last cigarette.
What’s the best way to check my heart disease risk?
Talk to your doctor about the ASCVD Risk Estimator. It uses your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking habits to calculate your 10-year risk. If you have a strong family history, ask about the Reynolds Risk Score, which adds CRP and family history for better accuracy.
Can genetic testing tell me if I’ll get heart disease?
Not definitively. While tests can identify genes like 9p21 or familial hypercholesterolemia, they only show increased risk-not certainty. Most heart disease is caused by lifestyle. Even with high genetic risk, healthy habits can reduce your chance by 50% or more. Genetics loads the gun; lifestyle pulls the trigger.
Next Steps: What to Do Today
If you’re reading this, you’re already ahead of most people. Now take action:- Write down your family’s heart health history-parents, siblings, grandparents.
- Book a checkup. Ask for blood pressure, cholesterol, and blood sugar tests.
- Track your steps. Aim for 7,000 a day. Use a free app or your phone.
- If you smoke, set a quit date. Call 1-800-QUIT-NOW or use the Smokefree app.
- Reduce salt. Swap processed snacks for fruits, nuts, or vegetables.
Heart disease doesn’t happen overnight. But neither does prevention. Small steps, repeated daily, change your future.

Ashley Karanja
Okay, I just read this and I’m sitting here with my matcha latte and my Apple Watch buzzing about my resting heart rate being ‘elevated’ (again). Like, I get it-arteries stiffen, estrogen drops, 9p21 variants are basically the universe’s passive-aggressive middle finger to your DNA-but what if you’re a 32-year-old woman who eats kale, runs 5Ks, and still has LDL higher than her ex’s emotional availability? 😅
Genetics isn’t destiny, but it’s the ghost in the machine. I had my dad’s familial hypercholesterolemia gene. My doctor said, ‘You’re not doomed, but you’re playing on expert mode.’ So I’m on a low-dose statin, tracking my CRP, and yes, I cry every time I see a donut. But I’m alive. And that’s the win.
Also-PM2.5? I live in L.A. My lungs feel like sandpaper. If we don’t fix air quality, no amount of kale will save us. This isn’t just personal-it’s systemic. And if you think healthcare access isn’t the real kicker? You haven’t tried getting a lipid panel without insurance. 💔
Karen Droege
Y’ALL. I’m a nurse in Vancouver and I’ve seen 27-year-olds with stents because they smoked, ate fast food every damn day, and thought ‘I’m young, I’m fine.’ NO. YOU’RE NOT.
That stat about 80% of heart disease being preventable? That’s not a statistic-it’s a scream from the ICU. I held a woman’s hand while she coded because she ignored her BP for 12 years. Her mom died at 52. She didn’t think it ran in the family because ‘Mom had high cholesterol, not a heart attack.’
Family history isn’t just ‘your uncle had a bypass.’ It’s your cousin who died at 38. It’s your sister who’s on 5 meds before she turned 40. STOP MINIMIZING. Start testing. Start moving. Start talking. Or you’ll be the next headline.
And yes, quitting smoking at 50? Still works. I’ve seen it. It’s not magic-it’s biology. Your endothelium remembers. And it forgives.
Also: SGLT2 inhibitors? GLP-1s? These aren’t just diabetes drugs-they’re heart saviors. Tell your doc. Demand them. Your future self will thank you. 🙏❤️
Shweta Deshpande
Hi everyone! I’m from India and I just wanted to say-this post made me cry. Not because I’m scared, but because I finally feel seen.
In my family, we think heart disease is ‘for fat old men who eat biryani every day.’ But my auntie? 54, thin as a stick, never smoked, ate only home-cooked food-and had a heart attack at 51. Turns out, she had silent diabetes. No symptoms. Just… gone.
Now I make my whole family get tested. Even my 28-year-old brother. He thinks he’s fine because he runs 10 minutes on the treadmill while watching Netflix. I told him: ‘Bro, that’s not exercise. That’s cardio theater.’ 😆
Walking 30 minutes? Yes. But also: stop eating fried samosas every Sunday. Swap tea for green tea. Sleep 7 hours. Your heart doesn’t care how ‘spiritual’ you are. It just wants to beat without screaming.
You got this. One step. One day. One swap. 💪❤️
Simran Kaur
As a desi woman who lost her dad to a heart attack at 56-he was a vegetarian, never drank, didn’t smoke-I’m here to say: genetics don’t care about your diet.
My dad had familial hypercholesterolemia. We didn’t know. No one tested. He just ‘felt tired.’ We thought it was stress from work. Turns out, his LDL was 380. That’s not ‘bad.’ That’s ‘emergency room with a defibrillator’ bad.
Now I nag my cousins. I send them links. I say: ‘Get your lipids checked. Even if you’re skinny. Even if you’re ‘healthy.’
And yes-air pollution in Delhi? It’s not just coughing. It’s arterial damage. Every breath is a tiny wound. We need policy change. But until then? N95 masks on bad days. Indoor plants. No open fires. Small things. Big impact.
I’m not angry. I’m just… tired of burying people too early. Let’s change that. 🌿
Neil Thorogood
So let me get this straight-you’re telling me I can’t just keep drinking protein shakes and doing 10 push-ups a day and call it ‘heart healthy’? 😂
Bro, I’ve been told I’m ‘low risk’ because I’m 35 and ‘not fat.’ But my BP is 142/90 and I’ve been smoking since college. And now I’m supposed to believe that walking 30 minutes will undo 15 years of nacho-fueled existential dread?
Here’s the truth: you don’t need to be perfect. You just need to stop being an idiot.
Quit smoking. Get tested. Move more. Eat less salt. Stop pretending you’re ‘too busy’ to care. Your heart doesn’t care about your hustle culture. It just wants to live.
And if you think ‘I’ll start next Monday’-you’re already lying to yourself. 🤡
Jessica Knuteson
Preventable? 80%? That’s the lie they sell you to make you feel guilty
Meanwhile the FDA approves drugs that raise BP and the food industry floods the market with HFCS and trans fats
It’s not about willpower
It’s about systems designed to kill you slowly
And now you’re supposed to blame yourself for not eating enough kale
Good luck with that
Also statins cause diabetes
So what’s the tradeoff again
Just sayin'
Angie Thompson
OMG I just did the ASCVD calculator and my 10-year risk is 19.8%. 😱
I’m 42, female, no family history, don’t smoke, walk every day, eat mostly plants-but my cholesterol is high and I’m prediabetic. I thought I was doing everything right. Turns out, I was doing ‘good enough’ and that’s not enough.
I’m booking my doctor’s appointment tomorrow. I’m asking for a coronary calcium scan. I’m trying the GLP-1 thing (if insurance lets me). I’m cutting out the almond croissants. I’m not going to wait for a heart attack to wake up.
And if you’re reading this and thinking ‘I’ll do it later’-I’m talking to YOU.
Tomorrow isn’t promised. But today? Today you can choose to live. 💕
Also-your heart doesn’t care how many yoga poses you do. It cares if you’re breathing clean air and sleeping 7 hours. Prioritize that. 🙏
rasna saha
I’m from rural India and we don’t have access to lipid panels or statins. But we do have turmeric, garlic, and walking 5 km to the market every day.
My grandmother lived to 92. She never saw a doctor. But she never ate processed food. She didn’t have a treadmill, but she weeded her garden every morning. She slept with the window open. She never stressed about ‘risk scores.’
Maybe the answer isn’t more tech. Maybe it’s less junk.
Simple things. Daily. Consistent.
That’s what saved her.
And maybe it can save us too.
James Nicoll
So let me get this straight-you’re telling me the entire medical-industrial complex is just selling us fear so we’ll buy pills and treadmills?
What if the real problem is that we’re all just… tired?
What if we’re not dying from bad cholesterol?
What if we’re dying from 12-hour workdays and no community and the constant pressure to be ‘productive’?
My dad died of a heart attack at 58. He worked 7 days a week. Never took vacation. Said ‘I don’t have time to be sick.’
Maybe the real risk factor isn’t smoking or salt.
Maybe it’s capitalism.
Just sayin’.
bella nash
It is imperative to note that the assertion regarding the preventability of heart disease is predicated upon an assumption of universal access to healthcare, nutritional literacy, and socioeconomic stability-conditions that are demonstrably non-universal.
Furthermore, the conflation of correlation with causation in the context of lifestyle interventions remains methodologically unsound.
The ASCVD estimator, while statistically robust, is not infallible and may yield false positives in populations with non-European ancestry.
One must exercise caution before adopting clinical recommendations derived from homogeneous datasets.
Epistemological humility is warranted.
Nicholas Miter
man i used to think i was fine til my bp was 150/95 at my 35 yr checkup
my doc said 'you're lucky you didn't drop dead at the gym'
i quit soda. started walking. took the statin. didn't even tell my friends
now my bp is 118/76
no medals. no trophies. just... not dead
weird how that works
Suresh Kumar Govindan
Cardiovascular disease is a tool of population control. The pharmaceutical industry profits from lifelong medication. The WHO promotes fear to justify surveillance. Genetic testing is a gateway to insurance discrimination. The ‘lifestyle’ narrative distracts from systemic poisoning by agrochemicals and EMF radiation. Your heart is not your enemy. The system is.
TONY ADAMS
bro i smoked for 20 years and now i’m 48 and my heart feels like a rusty bike chain
i quit last month
still feel like crap
but at least i’m not dead yet
thanks for the post
gotta keep going
Ashley Karanja
Just read Tony’s comment. I’m 4 months into quitting. Still get cravings when I smell coffee. Still feel like a ghost in my own body. But I held my niece’s hand yesterday and she said, ‘Auntie, your breath smells like flowers now.’
That’s the real win.
It’s not about stats or scans.
It’s about being here. For them.
Keep going, Tony. You’re not alone.