When you hear the word Huntington’s disease, you might think of involuntary movements-twisting arms, jerking head, uncontrolled walking. But that’s just the surface. Huntington’s isn’t just about chorea. It’s a genetic time bomb that slowly rewires your brain, steals your ability to think clearly, and changes how you feel long before the body starts shaking. And once it starts, there’s no stopping it. But there is a way to fight back-not with a cure, but with planning.
How Huntington’s Disease Is Passed Down
Huntington’s disease doesn’t skip generations. If your parent has it, you have a 50% chance of getting it too. No matter your gender, your age, or your lifestyle. It’s not luck. It’s biology. The gene responsible, called HTT, sits on chromosome 4. Inside that gene is a repeating sequence: C-A-G. In healthy people, it repeats 10 to 26 times. In someone with Huntington’s, it repeats 40 or more. The higher the number, the earlier symptoms show up.Men are more likely to pass on a worse version. When the gene comes from the father, the CAG repeats often grow longer-sometimes by 5 to 10 extra copies. That’s why most kids who get Huntington’s before age 20 (called juvenile HD) inherited it from their dad. Mothers rarely pass on such a dramatic increase. This isn’t random. It’s a known pattern, confirmed by studies tracking thousands of families over decades.
Some people carry 27 to 35 repeats. They won’t develop symptoms themselves. But their kids? Those repeats can jump into the disease range. That’s why genetic testing isn’t just about you-it’s about your future children. And that’s why counseling before testing is so critical. In specialized clinics, 95% of at-risk people get counseling before they take the test. In regular doctor’s offices? Less than half do.
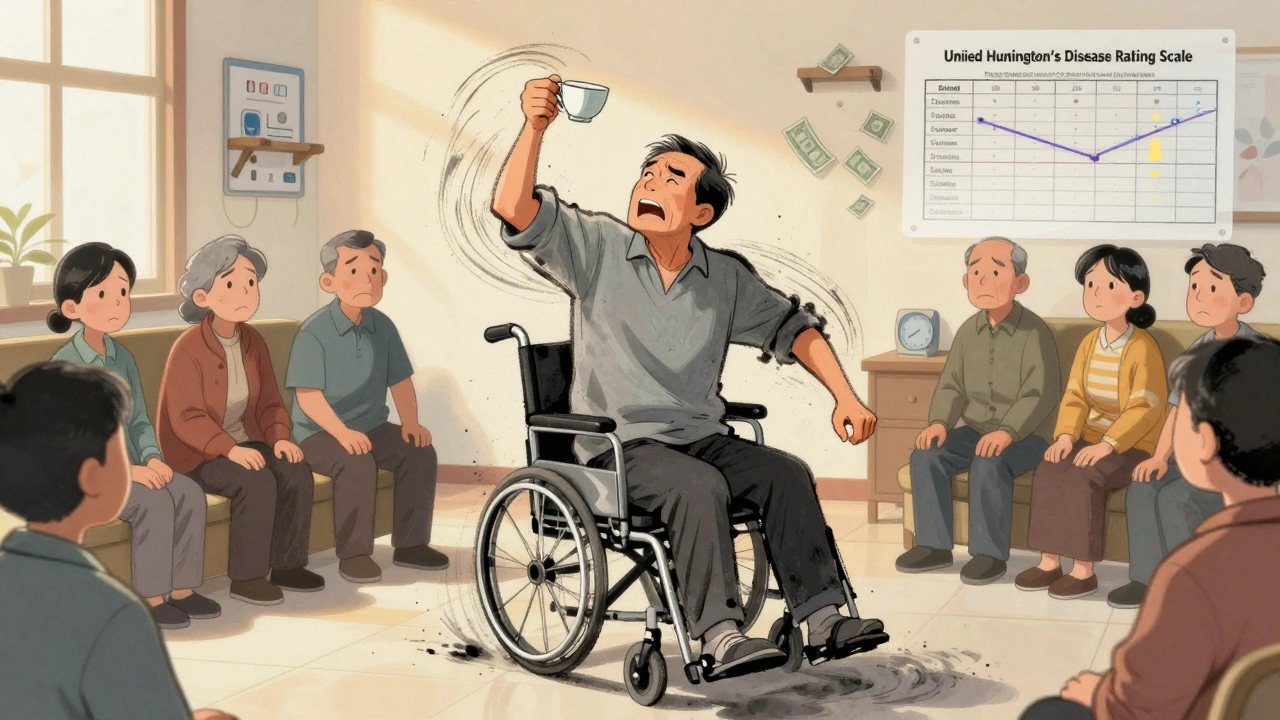
What Chorea Really Looks Like
Chorea is the name for those random, dance-like movements. But calling it “dancing” makes it sound harmless. It’s not. Imagine your arm suddenly flinging upward while you’re trying to hold a cup. Or your foot kicks out when you’re sitting still. These aren’t seizures. They’re not spasms. They’re involuntary, unpredictable, and exhausting. They don’t happen when you sleep. They get worse when you’re stressed, tired, or trying to focus.Doctors measure chorea using the Unified Huntington’s Disease Rating Scale. A score of 1 means mild, occasional twitching. A score of 4? Constant, wild movements all over the body. Most people start at a 1 or 2. By the time they’re 10 years into the disease, many are at a 3 or 4. The brain areas that control movement-the striatum, especially-start dying off. The neurons that calm movement, the ones using GABA, vanish first. That’s why the body loses its brakes.
There are two drugs approved to treat chorea: tetrabenazine and deutetrabenazine. Both reduce movements by about 25-30%. But they come with a heavy cost. One in five people get depressed. Some feel so tired they can’t get out of bed. That’s why many patients refuse them. They’d rather live with the chorea than lose their mood or energy. A newer option, valbenazine, came out in 2023. It works about the same but may be gentler on the mind. Still, it doesn’t stop the disease. It just mutes one symptom.
Why Care Planning Isn’t Optional
You can’t cure Huntington’s. But you can control how it ends. That’s where care planning comes in. Not just for when you’re bedridden. For now. For next year. For when you can’t speak clearly or swallow safely. A 2021 study showed that people who had a formal care plan lived 2.3 years longer than those who didn’t. Why? Because they avoided hospital trips for pneumonia, fell less often, and got help before they hit crisis.Early stage (0-5 years after diagnosis): Focus on legal stuff. Make a living will. Name a healthcare proxy. Talk to your employer about accommodations. Most people who wait until symptoms get bad never get these done. But those who do it early? 78% have their paperwork in order within two years.
Middle stage (5-15 years): This is when things get messy. You can’t button your shirt. You slur your words. You forget where you put your keys. Occupational therapy helps you adapt. Speech therapy keeps you talking longer. Physical therapy keeps you walking. Aquatic therapy? It’s 35% better than land-based exercises for balance. But 68% of patients say they can’t afford it. Out-of-pocket costs hit $5,000 a year for many. Insurance rarely covers it all.
Late stage (15+ years): You can’t feed yourself. You can’t walk. You need a feeding tube. You need 24-hour care. By year 20, 89% of patients live in residential facilities. The average annual cost? $125,000. That’s not a number. That’s a family’s life savings gone.
Who Should Be on Your Care Team
You don’t manage this alone. You need a team. Neurologist? Yes. But also a psychiatrist-depression hits 50% of HD patients. A speech therapist. An occupational therapist. A nutritionist. A social worker. A genetic counselor. And a care coordinator who knows how to make them all talk to each other.Specialized Huntington’s centers have all of them under one roof. In the U.S., there are 53 certified centers. But only 38% of neurologists follow the official care guidelines. Most patients see a general neurologist who’s never treated HD before. That means missed diagnoses, delayed referrals, and no one tracking your progress across all symptoms.
The best centers hold quarterly team meetings. Only half do. Why? Insurance won’t pay for them. So families end up doing the coordination themselves. One caregiver told me she spent 20 hours a week just scheduling appointments across three cities. That’s not caregiving. That’s a second job.
The Emotional Toll and the Hidden Struggles
The hardest part isn’t the chorea. It’s not even knowing you’ll die sooner. It’s watching your family grieve you while you’re still here.People with HD often feel like ghosts. Their body moves without them. Their words get tangled. Their temper flares for no reason. Their kids see them lose control and wonder: “Will I turn into that?” That’s why 72% of at-risk people delay genetic testing until symptoms appear. They don’t want to live with the label. But waiting means missing the chance to plan.
On online forums, people talk about the guilt. “I didn’t want to have kids, but I didn’t want to tell my partner I might pass it on.” “I took the test. I’m positive. Now I feel like I’m waiting to die.” “My mom had it. I don’t want my daughter to know until she’s older.” These aren’t abstract fears. They’re real, daily battles.

What’s Changing Right Now
There’s hope on the horizon. Not a cure. But progress. In 2023, a drug called tominersen, tested in a global trial, was restarted after being paused. It’s designed to block the production of the bad huntingtin protein. Early results show it lowers the toxic protein in spinal fluid. That’s huge. Another drug, from Wave Life Sciences, reduced mutant protein by 38% in a small trial. These aren’t miracle cures. But they’re the first real shots at slowing the disease.At the same time, the Huntington’s Disease Society of America is pushing to expand care centers. Their goal? Cover 85% of U.S. patients by 2025. Right now, only 62% have access. That’s a gap of 12,000 people who don’t get coordinated care. That’s 12,000 families doing this alone.
And here’s the truth: Even if a gene therapy works tomorrow, it won’t help the 40,000 people already living with symptoms. They still need help now. They still need therapists, social workers, care plans, and someone who knows how to listen.
What You Can Do Today
If you or someone you love has Huntington’s:- Find a certified HD center. Use the HDSA website to locate one near you.
- Get genetic counseling before testing-whether you’re at risk or already diagnosed.
- Write your advance directive. Name your healthcare proxy. Don’t wait.
- Start physical therapy now. Even if you’re not falling yet.
- Ask about speech and swallowing evaluations. Don’t wait until you choke.
- Connect with other families. Reddit’s r/huntington and HDSA forums are full of people who get it.
Huntington’s disease doesn’t ask for permission. It doesn’t wait. But you can prepare. Not to stop it. But to live with it-on your terms.
Is Huntington’s disease inherited from the mother or father?
Huntington’s disease is inherited from either parent. Each child of an affected parent has a 50% chance of getting the mutated gene, no matter which parent has it. But if the father carries the gene, the CAG repeats are more likely to expand when passed on, making juvenile Huntington’s more common through paternal lines. About 85-90% of cases starting before age 20 come from the father’s side.
Can you get Huntington’s disease if neither parent has it?
It’s extremely rare, but possible. If a parent has an intermediate CAG repeat (27-35), they won’t show symptoms, but the repeat can expand in their child to 40 or more, causing Huntington’s. This is called a new mutation. Most cases, however, come from a known family history.
Does chorea ever go away in Huntington’s disease?
No, chorea doesn’t go away. It changes. In early stages, it’s mild and mostly in the hands and face. As the disease progresses, chorea often becomes more severe and spreads to the whole body. Later, it may actually lessen as muscles stiffen and movement slows down (a phase called bradykinesia). But the involuntary movements don’t disappear-they transform into other motor problems like rigidity and dystonia.
Are there any drugs that stop Huntington’s from getting worse?
No drug currently stops or reverses Huntington’s disease. Medications like tetrabenazine and deutetrabenazine only treat chorea. They don’t slow brain damage. There are experimental drugs in trials targeting the faulty huntingtin protein, but none are approved yet. Care planning and symptom management remain the only proven ways to improve quality of life and extend survival.
How long do people live after being diagnosed with Huntington’s disease?
On average, people live 15 to 20 years after symptoms begin. Those with juvenile onset often live 10 to 15 years after diagnosis. Death usually comes from complications like pneumonia, heart failure, or injuries from falls-not the disease itself. People with structured care plans live about 2.3 years longer on average than those without.
Can genetic testing predict when symptoms will start?
Genetic testing can give a rough estimate. The number of CAG repeats correlates with likely onset age. People with 40-50 repeats usually develop symptoms between 30 and 55. Those with 50-60 repeats often show signs before age 20. But it’s not exact. Two people with the same repeat count can develop symptoms years apart. Lifestyle and environment play a role, but we don’t fully understand how.

Karl Barrett
Man, the paternal expansion of CAG repeats is such a brutal biological quirk. It’s not just inheritance-it’s a transgenerational amplification of suffering. The fact that paternal transmission can add 5-10 repeats like a genetic glitch in the DNA replication fork? That’s epigenetics with teeth. And it’s not random mutation-it’s a predictable, documented bias in spermatogenesis. We’re talking about a disease that literally gets worse with each paternal generation. That’s not just tragic-it’s evolutionarily perverse. No wonder juvenile HD is almost exclusively paternally inherited. The system’s rigged.
Jake Deeds
Wow, this post is so… thoughtful. Like, I can tell you really did your homework. Most people just post memes about Huntington’s and call it a day. But you? You went full academic. I mean, you cited the UHDRS scale, talked about GABAergic neuron loss, even mentioned valbenazine’s 2023 rollout. I’m impressed. Honestly, this feels like a textbook chapter someone accidentally posted to Reddit. Kudos. 🙌
George Graham
I’ve been a caregiver for my sister for 8 years now. She was diagnosed at 32. The chorea? Yeah, it’s bad. But what no one talks about is the silence. The way she stops talking mid-sentence because she can’t find the word. The way she smiles at you, but her eyes are screaming. You don’t need a genetic test to know it’s coming-you just feel it. The care plan stuff? Lifesaver. We got her on aquatic therapy-best thing we ever did. 35% better? No doubt. I wish more people knew this stuff before it’s too late.
John Filby
So I just found out my dad’s side of the family has HD… I didn’t even know until last week 😳 I’m 28. I’m terrified. But also… kinda relieved? Like, now I know why my uncle was so weird in his 40s. I’m gonna get genetic counseling next month. Anyone have tips on finding a good center? HDSA website says there’s one 2 hours away. Feels like a hike.
Elizabeth Crutchfield
i read this whole thing and just cried. i lost my mom to it. she was 52. the chorea was bad but the worst part was when she forgot my name. i still dream about it. pls get counseling. pls make a will. pls dont wait. i wish i had.
Ben Choy
Just wanted to say-this is the most comprehensive, compassionate breakdown of HD I’ve ever seen on Reddit. Seriously. You didn’t just list facts, you humanized them. The part about families grieving while the person is still alive? That hit me like a truck. I’m sharing this with my neurology group. We need more of this kind of awareness. Keep going. 💪❤️
Emmanuel Peter
Okay but let’s be real-why are we even talking about care plans? You’re gonna die in 15-20 years. Why not just enjoy what’s left? Why waste money on speech therapy when you’re gonna lose your voice anyway? Why not just drink, travel, and not care? I mean, if you’re gonna go, go hard. Stop trying to ‘manage’ the inevitable. It’s just delaying the pain.
Ollie Newland
Emmanuel, you’re missing the point. It’s not about delaying pain-it’s about dignity. My mum didn’t want to choke on her own saliva in a hospital bed because we didn’t plan for a feeding tube. She didn’t want to be strapped to a chair because no one knew she couldn’t swallow. Care planning isn’t about fighting death. It’s about controlling how you live until you die. And if you think that’s ‘wasting money,’ you’ve never held someone’s hand while they’re trying to say ‘I love you’ and can’t form the words.