Diuretic Selection Tool
Recommended Diuretic
Quick Takeaways
- Hydrochlorothiazide (HCTZ) is the most prescribed thiazide diuretic but isn’t always the strongest option.
- Chloro‑alidone offers about 1.5‑2× the blood‑pressure‑lowering potency of HCTZ.
- Indapamide combines diuretic action with vasodilation, making it useful for resistant hypertension.
- Metolazone works best when kidney function is reduced (eGFR<30ml/min).
- Choosing the right drug depends on dosing convenience, side‑effect profile, cost, and any co‑existing conditions.
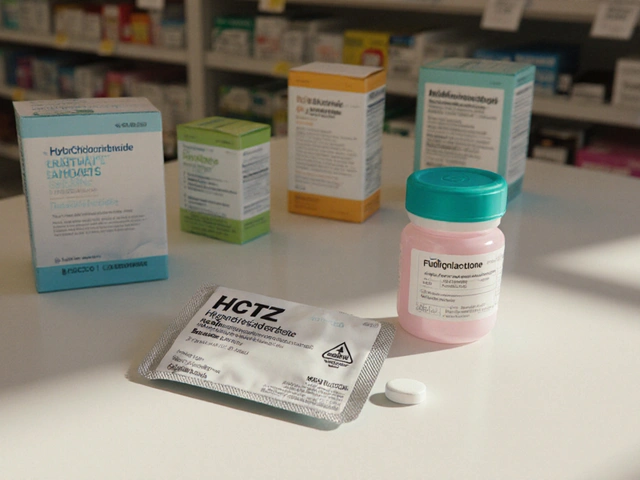
When you or a loved one needs a pill to tame high blood pressure, the name Hydrochlorothiazide probably shows up first. Hydrochlorothiazide has been on the market since the 1950s, works by nudging the kidneys to flush out excess salt and water, and costs almost nothing at the pharmacy. But “cheapest” doesn’t always equal “best”. Over the past decade, clinicians have started swapping it for newer or more potent thiazide‑like diuretics, especially when patients experience side effects or need tighter control.
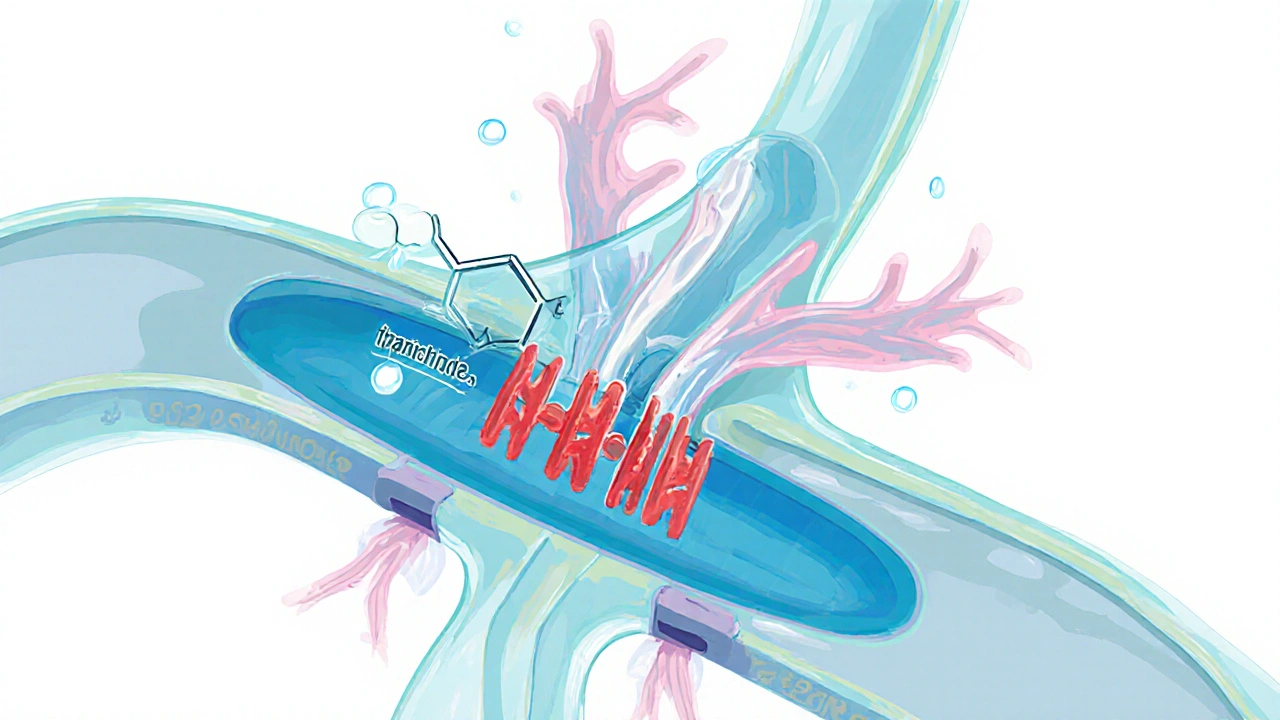
How Thiazide Diuretics Work
The class, known as Thiazide diuretic, works by blocking the sodium‑chloride transporter in the distal convoluted tubule. This reduces sodium reabsorption, pulls water out with it, and lowers blood volume - the main driver of a drop in systolic and diastolic pressure. The class also causes a mild dilation of peripheral vessels, adding to the antihypertensive effect. While the mechanism is shared, each drug differs in how long it stays active, how strongly it lowers pressure, and what side‑effects tend to appear.
Key Alternatives to Hydrochlorothiazide
- Chlorthalidone - Often called the “big brother” of HCTZ; half‑life of 40‑60hours.
- Indapamide - Combines diuretic power with direct vasodilation; available in an immediate‑release and a sustained‑release form.
- Metolazone - Retains activity at very low kidney function; usually paired with loop diuretics.
- Furosemide - A loop diuretic, not a thiazide, but sometimes used when HCTZ fails.
- Spironolactone - A potassium‑sparing diuretic that also blocks aldosterone; useful in resistant hypertension.
Side‑Effect Landscape
Because thiazides increase sodium loss, they also trigger potassium loss, uric acid rise, and sometimes higher blood sugar. Here’s how the alternatives compare:
- HCTZ - Common hypokalemia, occasional gout flare, modest rise in fasting glucose.
- Chlorthalidone - Similar electrolyte shifts but more pronounced; higher risk of hyponatremia.
- Indapamide - Lower incidence of potassium loss; less impact on glucose; can cause peripheral edema.
- Metolazone - Strong potassium depletion; may worsen gout.
- Furosemide - Potassium loss can be severe; ototoxicity at high doses.
- Spironolactone - Tends to raise potassium; may cause breast tenderness in men.
Cost and Accessibility (2025 UK Data)
Pricing in the UK follows the NHS drug tariff, but generic versions differ widely in the private market. Below is a snapshot of the average monthly cost for a typical dose in 2025.
| Drug | Typical Daily Dose | Half‑Life | Average Monthly Cost (NHS) | Common Side‑Effects |
|---|---|---|---|---|
| Hydrochlorothiazide | 12.5-25mg | 6-15h | £0.20 | Hypokalemia, gout |
| Chlorthalidone | 12.5-25mg | 40-60h | £0.45 | Hyponatremia, hypokalemia |
| Indapamide | 1.5mg SR | 14-18h | £0.60 | Edema, less potassium loss |
| Metolazone | 2.5-5mg | 8-10h | £0.70 | Severe hypokalemia |
| Furosemide | 20-40mg | 1.5-2h | £0.30 | Otodynia, electrolyte imbalance |
| Spironolactone | 25mg | 1.4h | £0.35 | Hyperkalemia, gynecomastia |
When to Choose Hydrochlorothiazide
If you’re starting treatment for uncomplicated stage1 Hypertension, HCTZ remains a solid first‑line choice. Its low cost, once‑daily dosing, and extensive safety data make it attractive for most adults without chronic kidney disease (CKD) or a history of gout. It also pairs well with ACE inhibitors or ARBs, a combo often recommended by NICE.
When Alternatives Shine
- Stronger blood‑pressure drop needed - Chlorthalidone often outperforms HCTZ by 5‑10mmHg in systolic reduction.
- Kidney function < 30ml/min/1.73m² - Metolazone retains efficacy where HCTZ loses grip.
- Risk of low potassium or gout - Indapamide’s milder effect on electrolytes can spare patients from frequent labs.
- Resistant hypertension - Adding low‑dose Spironolactone after a thiazide often normalizes pressure.
- Fluid overload or edema - Loop diuretic Furosemide clears volume faster but requires close monitoring.

Practical Decision‑Making Checklist
- Assess baseline kidney function (eGFR) and serum electrolytes.
- Identify comorbidities: gout, diabetes, heart failure.
- Consider cost and insurance coverage - NHS covers most, private patients may look at price differences.
- Start with the lowest effective dose; titrate up only if target <140/90mmHg isn’t reached after 4-6 weeks.
- Re‑check labs after 2 weeks, then at 3 months, focusing on potassium, sodium, uric acid, and glucose.
- If side‑effects emerge, switch to the next option on the list before adding a second antihypertensive.
Potential Pitfalls & How to Avoid Them
Many patients stop HCTZ because of “muscle cramps”. Those cramps are usually a sign of potassium loss. A simple solution is a low‑dose potassium supplement or swapping to Indapamide. Another common error is prescribing HCTZ alongside a non‑steroidal anti‑inflammatory drug (NSAID); the combo blunts the diuretic effect and can worsen kidney function.
Bottom Line
Hydrochlorothiazide remains a cost‑effective workhorse for initial hypertension therapy, but it’s not a one‑size‑fits‑all. Chlorthalidone, Indapamide, Metolazone, Furosemide, and Spironolactone each fill a niche when HCTZ falls short. By matching the drug’s pharmacokinetics, side‑effect profile, and price to the patient’s specific health picture, clinicians can achieve better blood‑pressure control with fewer hassles.
Frequently Asked Questions
Is Hydrochlorothiazide safe for long‑term use?
Yes, when monitored regularly. Most patients stay on it for years without serious issues, but annual checks of potassium, sodium, and kidney function are recommended.
Can I take Hydrochlorothiazide with my blood‑sugar medication?
Thiazides can raise blood glucose slightly, so people on insulin or sulfonylureas should have tighter glucose monitoring, especially during the first month.
Why do some doctors prefer Chlorthalidone over Hydrochlorothiazide?
Chlorthalidone has a longer half‑life, providing more consistent blood‑pressure control and a stronger reduction in cardiovascular events according to several meta‑analyses.
What should I do if I develop gout while on Hydrochlorothiazide?
Talk to your doctor about switching to Indapamide or adding a low‑dose colchicine. Reducing purine‑rich foods and staying hydrated also helps.
Is Spironolactone a good backup if Hydrochlorothiazide isn’t enough?
For resistant hypertension, a low dose of Spironolactone (12.5-25mg) added to a thiazide often brings pressure into target range, but potassium levels must be checked frequently.

zaza oglu
When you’re navigating the sea of diuretics, think of HCTZ as the reliable dinghy – it gets the job done for most patients, especially when eGFR is cruising above 60. But if you need a vessel that can also cut through resistant hypertension currents, Indapamide brings an extra sail of vasodilation to the mix. For those with tighter kidneys (eGFR 30‑60), Chloro‑alidone steps in as the sturdier craft, delivering roughly double the pressure‑dropping punch of HCTZ. In practice, the choice often hinges on kidney function, hypertension type, and how aggressively you need to lower that stubborn blood pressure.
Vaibhav Sai
Great breakdown! A quick grammar‑check note: the line if (eGFR = 60 && resistant) should be a double‑equals comparison (
==) to avoid assignment bugs. Also, consider adding a tooltip explaining why Indapamide’s vasodilatory effect matters for resistant cases – it can help clinicians remember the mechanistic edge without digging through pharmacology texts. Minor code tweaks like these make the tool both safer and more user‑friendly.Lindy Swanson
Honestly, I’m not convinced the tool’s logic is as solid as it claims. The condition
if (eGFR = 60 && resistant)will always fire for any eGFR because it’s an assignment, not a comparison. That means everybody gets Indapamide, even those with normal kidneys who might be better off on HCTZ. It’s a classic case of over‑engineered “smart” UI that actually misguides prescribers.Crystal Heim
What a simplistic presentation. The tool lumps together vastly different patient scenarios without accounting for electrolyte profiles or comorbidities. A seasoned clinician knows you can’t just pick a diuretic based on eGFR alone; potassium handling, uric acid levels, and even patient adherence matter. The lack of nuance makes this feel like a one‑size‑fits‑all cheat sheet.
Sruthi V Nair
The philosophical angle here is fascinating: we’re reducing complex human physiology to a handful of variables, essentially quantifying what is inherently qualitative. Yet, that reductionism can empower clinicians to make faster decisions when time is scarce. It’s a delicate balance between oversimplification and practical utility; the tool leans toward the latter, offering a scaffold rather than a final verdict.
Mustapha Mustapha
I’ve seen similar calculators in practice, and they’re handy when you need a quick cross‑check. The key is to remember they’re adjuncts – not replacements for clinical judgment. If you’re comfortable with the pharmacology, the tool can save a few keystrokes; otherwise, double‑check the recommendations against the patient’s full medication list.
Ben Muncie
One sentence: Indapamide isn’t a magic bullet.
Greg DiMedio
Wow, another “cutting‑edge” web widget that pretends to replace a decade of medical training. Sure, it spits out a name, but does it factor in the patient’s lifestyle, the cost of medication, or the fact that some doctors still swear by bendroflumethiazide? I guess if you love shiny buttons more than solid evidence, this is for you.
Badal Patel
Esteemed colleagues-might I draw attention to the theatrical flaw in the script? The conditional
if (eGFR = 60 && resistant)is, dare I say, a glaring mis‑assignment!; behold, the logic will ever‑so‑gracefully declare Indapamide universally, irrespective of renal nuance. Such a misstep, though minute in code, resonates profoundly across clinical decision‑making, echoing the perils of unchecked automation. Shall we not aspire to a more rigorous algorithm, one that respects both mathematics and medicine?Kara Guilbert
Ths tool is gud but i
Sonia Michelle
From a philosophical standpoint, the tool embodies the principle of “rule‑based heuristics”: it offers a structured pathway while leaving room for the practitioner’s moral responsibility. That said, integrating patient preferences-like aversion to frequent urination-could elevate its ethical grounding. In short, it’s a solid start, but remember to blend algorithmic advice with human empathy.
Neil Collette
Ah, the glorious dance of code and pharmacology – a ballet where the choreographer forgot the steps. First, the script’s assignment operator masquerades as a comparison, sending every patient straight to Indapamide, regardless of whether their kidneys are a delicate blossom or a sturdy oak. Second, the absence of electrolyte considerations turns this calculator into a one‑dimensional oracle, blind to potassium, sodium, and uric acid – the silent actors in hypertension’s drama. Third, the UI’s glowing result box gives the illusion of certainty, while beneath lies a quagmire of unchecked assumptions. Fourth, developers seem to think that eGFR alone dictates diuretic potency, ignoring the nuanced interplay of dose‑response curves and patient adherence. Fifth, the tool’s static text fails to adapt to comorbidities such as diabetes or heart failure, where loop diuretics might be preferable. Sixth, it offers no pathway for clinicians to input current medication lists, a glaring omission for anyone aware of drug‑drug interactions. Seventh, the code’s readability is hampered by inconsistent spacing, making future maintenance a nightmare for any sane programmer. Eighth, the use of innerHTML without sanitization opens a modest security hole that could be exploited in a less reputable environment. Ninth, the tool’s aesthetic flair, while appealing, masks the underlying scientific rigor that should be front‑and‑center. Tenth, the lack of references or citations leaves the user stranded, forced to trust an algorithm that offers no provenance. Eleventh, the decision thresholds (eGFR ≥ 30, < 60) are arbitrarily chosen without justification from clinical guidelines. Twelfth, the static message “Enter your patient data and click Analyze” is a placeholder that betrays an unfinished product. Thirteenth, the entire endeavor feels like a vanity project for a developer eager to show off JavaScript tricks rather than solve a genuine clinical need. Fourteenth, the perpetual reliance on a web browser’s JavaScript engine makes the tool vulnerable to ad‑blockers or script‑blocking extensions, potentially rendering it useless in practice. Fifteenth, and perhaps most damning, is the moral hazard: clinicians might lean on this simplistic widget, sidelining their own critical thinking, and ultimately compromising patient care. In sum, while the concept is noble, the execution is riddled with oversights that demand urgent remediation.