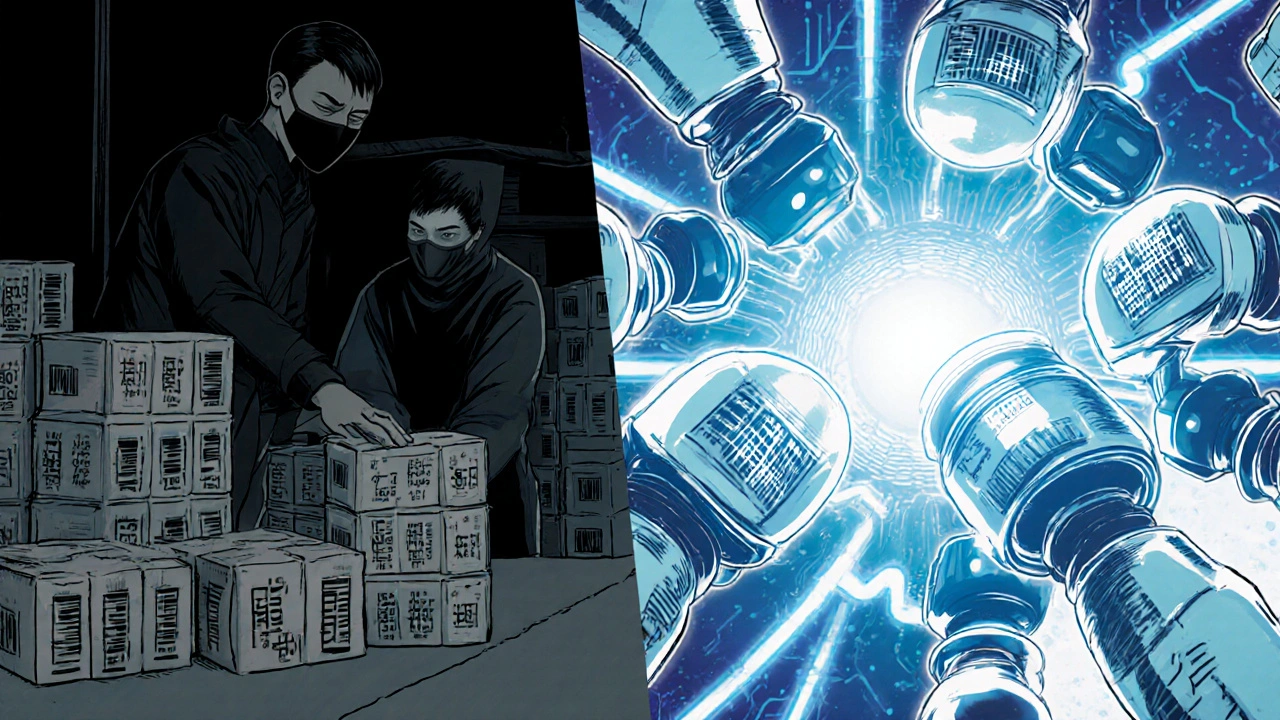
Every pill, every vial, every box of medicine you buy should be traceable. If it’s not, it could be fake. And fake drugs kill. In 2023, the WHO estimated that 1 in 10 medical products in low- and middle-income countries are substandard or falsified. In high-income countries, it’s rarer-but not gone. The difference between a life saved and a life lost often comes down to two things: a lot number and a serial code.
What’s the difference between a lot number and a serial code?
A lot number tracks a group. Think of it like a batch of cookies baked in the same oven, at the same time, with the same ingredients. If one cookie is spoiled, you pull that batch. That’s lot tracking. Lot numbers usually include the production date, shift, location, and raw material batch. They’re assigned to hundreds or thousands of identical units. A serial code is different. It’s like a fingerprint for a single unit. Every box of insulin, every bottle of antibiotics, every pacemaker gets its own unique serial number. No two are the same. Serial codes track the journey of one specific item from factory to pharmacy to patient. In the fight against counterfeit drugs, both matter. Lot numbers help find where bad medicine came from. Serial codes prove that the exact bottle in your hand is real.Why track-and-trace is the only way to stop fake medicine
Before digital tracking, recalls were messy. If a batch of blood pressure pills was found to have the wrong ingredient, manufacturers had to pull every single pill they’d ever made. That cost millions. It wasted real medicine. And patients still couldn’t be sure if their bottle was safe. Now, with lot and serial tracking, it’s precise. When the FDA got a report in 2023 that a batch of metformin contained a cancer-causing impurity, they didn’t shut down every pharmacy. They scanned the lot number on the bottles. Only 14,000 bottles out of 2.3 million were affected. The rest stayed on shelves. Patients kept taking their medicine. The recall cost 63% less than a full-line pull. Serial codes add another layer. In the EU, every prescription medicine box now has a 2D barcode with a unique serial number. When you buy it, the pharmacy scans it. If the system says it’s fake, or already sold, the transaction blocks. No sale. No fake drug in your hands. This system, called the Falsified Medicines Directive, went live in 2019. Since then, over 2 billion medicine packages have been verified in Europe. Only 0.002% were flagged as suspicious. That’s not zero-but it’s a massive drop.How it works in real life
Here’s how it plays out on the ground:- A drugmaker produces 50,000 bottles of amoxicillin. They assign them all to lot number B20250417-03 (April 17, 2025, shift 3).
- Each bottle gets its own serial code: S984723102984732.
- The bottles ship to a distributor, then to a regional warehouse, then to a pharmacy.
- At every stop, the lot number and serial code are scanned and logged into a secure digital system.
- If a patient reports a bad reaction, the pharmacy scans the bottle. The system shows the lot number. The manufacturer checks: were there other reports from that same batch? Did the temperature spike during shipping? Was the serial code ever used before?
What happens when the system fails
It’s not perfect. Failures happen when people cut corners. In 2023, a small U.S. pharmacy was fined $850,000 by the FDA. They were using old manual logs. They’d write lot numbers by hand on sticky notes. One note got lost. Another was smudged. When a recall came in, they couldn’t tell which bottles they’d sold. They had to destroy 900 bottles-even though only 12 were in the bad batch. Another case: a distributor in Florida started skipping scans to save time. They’d scan every 10th bottle, assuming the rest were fine. One fake drug slipped through. It ended up in a nursing home. Two elderly patients died. The company was shut down. The lesson? Technology alone won’t save you. Discipline will. Every bottle, every scan, every log must be treated like a legal record. Because it is.Who’s required to use it?
In the U.S., the Drug Supply Chain Security Act (DSCSA) requires full track-and-trace for prescription drugs by 2023. That means every manufacturer, repackager, wholesaler, and pharmacy must scan and record lot and serial numbers at every handoff. The EU’s Falsified Medicines Directive is even stricter. Every prescription medicine must have a unique serial code and a tamper-evident seal. Pharmacists must verify each one before dispensing. Even over-the-counter drugs are starting to get tracked. In 2025, the FDA began requiring serial codes on all pain relievers sold in bulk to pharmacies. Why? Because counterfeit Tylenol and ibuprofen are still being made in labs overseas-and shipped in fake packaging that looks real. The global market for track-and-trace systems is now worth over $3.8 billion. It’s growing fast. Why? Because regulators are watching. And patients are demanding safer medicine.
What’s next for track-and-trace?
The next big step? Real-time monitoring. Some pharmaceutical companies are now putting tiny temperature sensors inside shipping boxes. If the medicine gets too hot or too cold during transit, the system alerts the pharmacy before the box even arrives. That’s huge for insulin, vaccines, and biologics. Blockchain is being tested too. Instead of one company controlling the data, multiple parties-manufacturer, shipper, pharmacy-each hold a copy. If someone tries to fake a serial code, the system knows instantly. And AI? It’s starting to predict where fake drugs might show up. By analyzing shipping routes, payment patterns, and online sales, AI models can flag high-risk distributors before a single fake bottle is sold. None of this is science fiction. It’s happening now.What you can do as a patient
You don’t need to be a tech expert. But you can protect yourself.- Always ask your pharmacist to scan your prescription. If they say they don’t, ask why.
- Check the packaging. Is the lot number printed clearly? Is the serial code on a sticker or engraved? Fake drugs often have blurry, smudged, or missing codes.
- Don’t buy medicine from websites that don’t require a prescription. If it’s too cheap, it’s likely fake.
- Report anything suspicious. The FDA has a portal for reporting counterfeit drugs. One report could save a life.
Are lot numbers and serial codes the same thing?
No. A lot number identifies a group of products made together under the same conditions-like a batch of 10,000 bottles of the same drug. A serial code is a unique identifier for a single unit, like one specific bottle. Lot numbers help with batch recalls; serial codes prove the exact item is authentic.
Can I check if my medicine is real using the lot or serial number?
In many countries, yes. In the EU, you can scan the 2D barcode on prescription medicine packaging with a smartphone app to verify it’s legitimate. In the U.S., you can call the manufacturer’s toll-free number or visit their website and enter the lot and serial number. If the system says it’s not registered or already sold, the drug may be counterfeit.
Why do some drugs have serial codes and others don’t?
Regulations require serial codes for prescription drugs in the U.S. and EU. Over-the-counter medicines like painkillers are starting to get them too, but not all are required yet. High-risk or high-value drugs-like insulin, cancer meds, or antibiotics-are prioritized. Cheap generics or non-prescription items may still use only lot numbers.
What happens if a pharmacy doesn’t scan my medicine?
In the U.S. and EU, pharmacies are legally required to scan prescription drugs before dispensing. If they don’t, they’re breaking the law. It also puts you at risk. Without scanning, they can’t detect if the drug is expired, recalled, or fake. Always ask them to scan it. If they refuse, report it to your state board of pharmacy or the FDA.
Is track-and-trace foolproof against counterfeit drugs?
No system is 100% foolproof. But track-and-trace has cut counterfeit medicine circulation by more than 70% in regulated markets. Fake drugs now mostly come from illegal online pharmacies or unregulated supply chains. The system makes it extremely hard for counterfeiters to slip real-looking drugs into the legal pipeline. It’s the best tool we have-and it’s getting better.


Gary Hattis
Man, I never thought about how much goes into making sure your Tylenol isn’t made in a basement in Bangladesh. The lot number thing? It’s like a birth certificate for your meds. And serial codes? That’s the fingerprint. If your insulin has a serial, and it’s been scanned at every stop, you’re basically getting a tamper-proof guarantee. This isn’t just tech-it’s survival.
Esperanza Decor
I work in a pharmacy and we scan every script. It’s not just policy-it’s peace of mind. Last month, a patient came in with a bottle from some sketchy online seller. We scanned it. System flagged it as ‘already dispensed’ in Ohio. Turned out it was stolen. We called the cops. That’s the system working.
Shante Ajadeen
This is actually one of the most reassuring things I’ve read in a while. Knowing that someone’s checking every bottle before it gets to me? That’s the kind of detail that makes me trust the system. Thanks for laying it out so clearly.
Johnson Abraham
lol so now my tylenol has a serial number? next theyll put gps in my advil. why do we need this? i just wanna feel better. also i think the fda is just trying to sell more scanners. 🤡
Benjamin Stöffler
One must pause and consider the ontological implications of serialization in pharmaceuticals: if a pill is uniquely identifiable, does its identity precede its existence-or is it merely a construct of bureaucratic epistemology? The lot number, a collective signifier, represents the Hegelian synthesis of mass production; the serial code, the Kantian noumenon of individuality. Yet, when the system fails-as it did in Ohio, where the temperature sensor failed to log a 12-hour spike at 47°C-do we not confront the absurdity of trusting algorithmic certainty over human fallibility? The answer, I submit, lies not in the code, but in the discipline to scan, to log, to verify-even when no one is watching. And yet… who watches the watchers?
Erica Cruz
Let’s be real-this whole system is a money grab. The FDA doesn’t care about your safety; they care about vendors selling $200k scanning terminals to every pharmacy. And don’t get me started on blockchain-another buzzword to justify corporate bloat. Meanwhile, real problems like drug pricing? Ignored. This is theater. With barcodes.
Deepa Lakshminarasimhan
you ever think maybe the whole thing is rigged? like… what if the serial numbers are fake too? what if the system is just another way for big pharma to track you? i heard they’re linking it to your insurance. and the ‘verified’ label? it’s just a sticker. anyone can print that. the real fake drugs? they’re already in the system. they just don’t get flagged… because they’re paid for.
Renee Ruth
Two elderly people died because someone skipped scans. TWO. And now we’re talking about blockchain? That’s not innovation-that’s a funeral with a PowerPoint. The system isn’t broken. The PEOPLE are. And until we start holding individuals accountable-not just companies-this will keep happening. Someone lost their mom. And you’re all talking about barcodes like it’s a TED Talk.
Elizabeth Buján
I just want to say thank you for writing this. I’ve been scared to buy meds online since my aunt got sick from fake antibiotics. It’s not just about safety-it’s about dignity. You deserve to trust your medicine. And this system? It’s the closest thing we’ve got to a promise that someone out there cares enough to make sure you don’t get poisoned. That matters.
Charles Lewis
It is imperative to recognize that the implementation of track-and-trace protocols represents not merely a logistical advancement, but a profound ethical commitment to public health. The convergence of regulatory frameworks such as the DSCSA and the Falsified Medicines Directive reflects a global consensus on the non-negotiable value of pharmaceutical integrity. Moreover, the integration of temperature-sensitive IoT devices within supply chains signifies a paradigm shift from reactive to predictive safety modeling. One must also acknowledge the latent potential for AI-driven anomaly detection to preemptively identify high-risk distribution nodes-thereby transforming the supply chain from a linear conduit into a dynamic, self-correcting network. The cost of non-adoption, as evidenced by the Florida incident, is measured not in dollars, but in lives. We are not merely scanning barcodes; we are safeguarding human dignity.
Danae Miley
Correction: The FDA began requiring serial codes on all pain relievers sold in bulk to pharmacies in 2024-not 2025. The original text contains a factual error. This is critical. Accuracy matters when lives are at stake. Please correct it.
Samantha Wade
This is exactly the kind of clarity we need. People think this is just paperwork-but it’s armor. Every scan is a shield. Every log is a promise. And yes, it’s a lot. But when you’re holding your kid’s asthma inhaler or your grandpa’s heart meds-you don’t want to hope it’s real. You want to know. Thank you for making this real.
dace yates
Wait-so if I scan my bottle and it says ‘already sold,’ does that mean someone else already used it? Or could it just be a glitch? What if the pharmacy scanned it by accident? Is there a way to appeal? I’m just trying to understand how foolproof this really is.