Imagine your body is a house. One leaky pipe? Fix it. A flickering light? Replace the bulb. But what if five things go wrong at once - the wiring’s frayed, the furnace is overworking, the gutters are clogged, the foundation’s sinking, and the smoke alarm won’t stop beeping? You wouldn’t just patch each problem separately. You’d call in a pro to see what’s really going on. That’s what metabolic syndrome is: five warning signs showing up together, screaming that your body’s systems are out of balance - and your heart is in danger.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t a single disease. It’s a cluster of five related conditions that, when they happen together, dramatically raise your risk of heart disease, stroke, and type 2 diabetes. You don’t need to have all five - just three of them - and you’re diagnosed. These aren’t random quirks. They’re signs your body’s metabolism is stuck in a harmful cycle, mostly driven by insulin resistance. The five diagnostic markers are clear-cut:- Abdominal obesity: Waist size over 40 inches (102 cm) for men, or 35 inches (88 cm) for women. For Asian populations, the thresholds are lower - 35 inches for men, 31 inches for women - because fat around the belly is more dangerous at smaller sizes.
- High triglycerides: 150 mg/dL or higher. These are fats in your blood that, when too high, clog arteries.
- Low HDL cholesterol: Below 40 mg/dL for men, below 50 mg/dL for women. HDL is the "good" cholesterol that helps clean out artery gunk. When it’s low, cleanup crews are undermanned.
- High blood pressure: 130/85 mmHg or higher. That’s not just "a bit high" - it’s a signal your heart is working too hard against stiff, narrowed vessels.
- High fasting blood sugar: 100 mg/dL or higher. This isn’t diabetes yet, but it’s your body’s red flag that insulin isn’t doing its job.
These numbers aren’t arbitrary. They come from decades of research, including the Framingham Heart Study and the National Health and Nutrition Examination Survey (NHANES). The data shows that having three or more of these factors doubles your risk of heart disease and makes you five times more likely to develop type 2 diabetes.
Why It’s More Than Just a List of Problems
The real danger isn’t that you have high blood pressure or high sugar. It’s that they’re all happening at once - and feeding each other. The engine behind this mess is insulin resistance. Your cells stop responding properly to insulin, the hormone that shuttles glucose into muscle and fat cells for energy. So your pancreas pumps out more insulin to compensate. That extra insulin doesn’t just raise blood sugar - it also makes your liver churn out more fat, tightens your blood vessels, and causes your kidneys to hold onto sodium, which spikes blood pressure. And here’s the kicker: belly fat - especially the deep, visceral kind around your organs - isn’t just storage. It’s active tissue that releases inflammatory chemicals. These chemicals make insulin resistance worse, which makes fat storage worse, which makes inflammation worse. It’s a loop with no off switch. This is why treating each condition alone - like popping a pill for blood pressure or statins for cholesterol - doesn’t fix the root problem. You’re treating symptoms, not the cause. The American Heart Association calls this syndrome a "clinical warning sign," not just a checklist. It’s your body’s SOS signal.Who’s Most at Risk?
About one in three American adults has metabolic syndrome - that’s over 86 million people. But it’s not evenly spread. The risk jumps with age: only 20% of people in their 20s and 30s have it, but nearly half of those over 60 do. Ethnicity matters too. Hispanic adults have the highest rates (38.6%), followed by non-Hispanic Black (31.8%) and non-Hispanic white (34.2%) adults. Asian Americans develop the syndrome at lower body weights, which is why their waist thresholds are lower. Obesity is the biggest driver. Since 2000, abdominal obesity in U.S. adults has climbed from 46% to nearly 60%. But it’s not just about weight. People with polycystic ovary syndrome (PCOS), sleep apnea, or a family history of type 2 diabetes are at much higher risk. Even if you’re "normal weight," if you carry fat around your middle, you’re still vulnerable. And here’s something many don’t realize: metabolic syndrome is now responsible for 75-80% of new type 2 diabetes cases. It’s the main pathway from prediabetes to full-blown disease.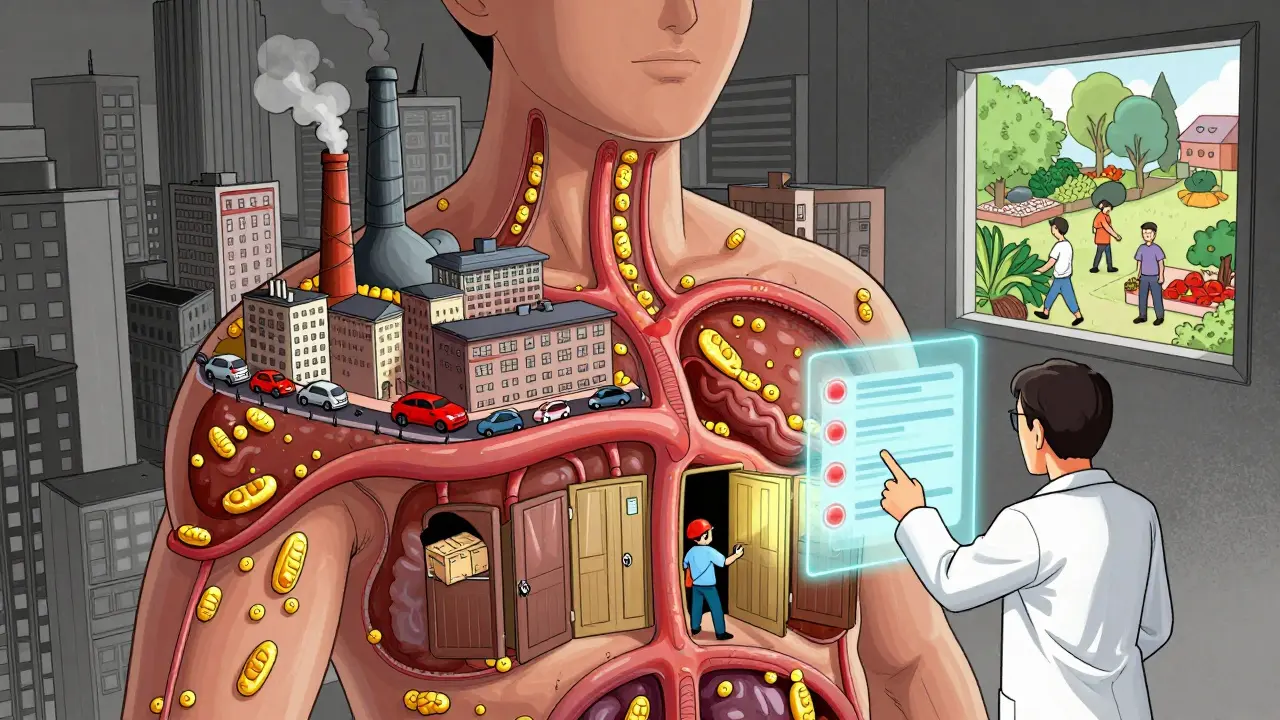
How It’s Diagnosed - And Why Many Miss It
Doctors don’t usually screen for metabolic syndrome automatically. Most patients are diagnosed only after being tested for one of the five components - say, high cholesterol during a routine checkup. But here’s the problem: 68% of people on health forums like HealthUnlocked say their doctor never connected the dots. One person might be treated for high blood pressure. Another for high triglycerides. But no one says, "You’ve got three of the five markers. You’ve got metabolic syndrome. Let’s fix this before it breaks your heart."Proper diagnosis requires more than a single blood test. It needs:
- Accurate waist measurement (not just weight on a scale)
- Fasting blood tests for glucose and lipids
- Multiple blood pressure readings over time (not just one office reading)
- Sometimes an oral glucose tolerance test if fasting sugar is borderline
Many primary care providers simply don’t have the time or training to piece it all together. That’s why patients often fall through the cracks - until they have a heart attack or get diagnosed with diabetes.
What Actually Works to Reverse It
The good news? Metabolic syndrome is reversible. And you don’t need surgery or expensive drugs. The most powerful treatment is lifestyle change - the same kind proven in the Diabetes Prevention Program (DPP), which followed over 3,000 people at high risk for diabetes. The DPP showed that losing just 7% of your body weight - say, 15 pounds if you weigh 215 - and getting 150 minutes of brisk walking per week cuts your risk of developing diabetes by 58%. Over 10 years, intensive lifestyle changes reduced metabolic syndrome by 41% compared to placebo. What does that look like in real life?- Move more: 30 minutes a day, five days a week. Doesn’t have to be gym workouts. Gardening, dancing, walking the dog - all count.
- Eat smarter: Cut back on sugar, refined carbs, and processed foods. Focus on vegetables, lean protein, whole grains, nuts, and healthy fats like olive oil and avocado. Aim for 1,200-1,500 calories a day for women, 1,500-1,800 for men.
- Sleep better: Poor sleep worsens insulin resistance. Aim for 7-8 hours.
- Manage stress: Chronic stress raises cortisol, which increases belly fat and blood sugar.
People who stick with it report big wins: blood pressure dropping, triglycerides halving, waistlines shrinking by 3-5 inches in six months. One Reddit user lost 12% of his body weight and reversed three of his five markers. Another, with PCOS, said her periods returned and her energy came back after six months of consistent changes.

Where the System Fails - And How to Fight Back
The biggest barrier isn’t willpower. It’s the healthcare system. Most insurance plans don’t cover structured lifestyle programs. Only 28% of Medicare Advantage plans pay for evidence-based diabetes prevention programs. So even if your doctor says, "Try the DPP," you might not be able to access it. That’s why community programs matter. The CDC’s National Diabetes Prevention Program uses trained coaches - often lay health workers - to guide people through lifestyle changes. In one study, Hispanic participants in these programs lost more weight than those in standard care. And now, technology is helping. In January 2023, the FDA approved the first digital therapeutic for metabolic syndrome: DarioHealth’s Metabolic+ app. It combines continuous glucose monitoring with daily coaching. In a trial, users reduced their HbA1c by 0.6% and waist size by 3.2 cm in just six months. But no app replaces human support. The most successful outcomes come from multidisciplinary teams: a dietitian, a physical therapist, a behavioral counselor, and a doctor who coordinates care. Mayo Clinic’s program saw 68% of participants achieve remission after 12 months.What’s Next - And Why There’s Hope
Metabolic syndrome is growing fast. By 2030, nearly 40% of the world’s adults may have it. But it’s also one of the most preventable conditions. The DiRECT trial in the UK showed that with intensive weight loss (15+ kg), 46% of people with type 2 diabetes and metabolic syndrome went into full remission - meaning their blood sugar returned to normal without medication. New research is diving deeper into genetics. Variants in genes like PNPLA3 and TM6SF2 can predict who responds best to diet versus exercise. The NIH is funding $25 million for precision medicine approaches to match people with the right intervention. The American College of Cardiology now recommends that people with metabolic syndrome start statins earlier, even if their cholesterol isn’t sky-high. Why? Because the syndrome itself is now recognized as an independent risk enhancer - a signal that your arteries are under siege. This isn’t about fear. It’s about power. You don’t need to wait for a diagnosis to act. If you’re carrying extra weight around your middle, have high blood pressure, or feel constantly tired after meals, start now. Walk after dinner. Swap soda for water. Sleep an extra hour. These aren’t "diet changes." They’re life-saving habits.Can You Really Reverse It?
Yes. Not always completely, but often enough to avoid heart attacks, strokes, and diabetes. The key is catching it early - before the damage becomes permanent. The body is incredibly adaptive. When you remove the triggers - excess sugar, inactivity, chronic stress - it starts to heal itself. Insulin sensitivity improves. Inflammation drops. Blood pressure comes down. HDL rises. It’s not about perfection. It’s about consistency. One person I know lost 30 pounds over 18 months. She didn’t do keto or juice cleanses. She just started eating vegetables with every meal, walked 20 minutes after dinner, and stopped drinking sugary coffee. Within six months, her triglycerides dropped from 280 to 110. Her blood pressure went from 142/90 to 118/76. She didn’t need pills. She just changed her daily rhythm. Metabolic syndrome isn’t a life sentence. It’s a wake-up call. And the best part? You don’t need a doctor’s permission to answer it.Can you have metabolic syndrome and not be overweight?
Yes. While abdominal obesity is one of the five criteria, it’s possible to have insulin resistance and other metabolic issues even if your overall weight is normal. This is sometimes called "TOFI" - thin outside, fat inside. Visceral fat around organs can be high even in people with a normal BMI, especially if they’re inactive or eat a lot of processed carbs. Waist measurement is a better indicator than scale weight.
Are medications used to treat metabolic syndrome?
There’s no single drug approved to treat metabolic syndrome as a whole. But doctors often prescribe medications for individual components: statins for cholesterol, ACE inhibitors or beta-blockers for blood pressure, metformin for high blood sugar. These help manage symptoms, but they don’t reverse the root cause - insulin resistance. Lifestyle change remains the only proven way to reverse the syndrome.
How long does it take to reverse metabolic syndrome?
Significant improvement can happen in as little as 6 months with consistent lifestyle changes. Studies show that losing 5-7% of body weight and exercising 150 minutes per week leads to reductions in waist size, blood pressure, and triglycerides within that timeframe. Full remission - where all five criteria fall below diagnostic thresholds - often takes 12-18 months, but it’s achievable.
Does metabolic syndrome increase stroke risk?
Yes. The same factors that cause heart disease - high blood pressure, insulin resistance, inflammation, and abnormal fats in the blood - also damage blood vessels in the brain. People with metabolic syndrome have a significantly higher risk of ischemic stroke, which occurs when a clot blocks blood flow to the brain. Managing the syndrome reduces this risk as much as it reduces heart attack risk.
Is metabolic syndrome the same as prediabetes?
No, but they often go together. Prediabetes means your blood sugar is higher than normal but not high enough for a diabetes diagnosis. Metabolic syndrome includes prediabetes as one of its five components, but it also requires two other factors - like high blood pressure or low HDL. You can have prediabetes without metabolic syndrome, and vice versa, but having both means your risk is much higher.


Shelby Price
This is such a clear breakdown. I never realized how connected all these factors are. Just last month my doc mentioned my waist size and triglycerides, but never said it was a syndrome. Feels like I got handed a flashlight in a dark room.
Geri Rogers
I reversed mine in 8 months just by walking after dinner and swapping soda for sparkling water. No keto, no supplements. Just consistency. My BP dropped 20 points. 🙌 You don’t need to be perfect, just persistent.
Alex LaVey
I’ve seen this play out in my family. My dad had all five markers but refused to change. Said he was "too old to start over." Two years later, he had a stroke. Don’t wait for the emergency room to wake you up. Start small. Today. Right now.
Alec Stewart Stewart
I’m 32, normal weight, but my waist is 36 inches. My doc laughed when I asked if I could have metabolic syndrome. Turns out I did. Three markers. Now I do 20 min walks after dinner and eat veggies with every meal. My energy is back. 💪
Demetria Morris
People who don’t take this seriously are just being selfish. Your poor choices affect everyone around you - your kids, your spouse, your insurance premiums. Stop pretending it’s just about looks.
Nathan King
The clinical nomenclature of metabolic syndrome has been systematically underutilized in primary care settings due to structural time constraints and reimbursement models that incentivize pharmacological intervention over behavioral modification. The paradigm shift required is both epistemological and institutional.
rahulkumar maurya
You think this is bad? In India, we have a whole generation of kids with visceral fat and high fasting glucose because of milk tea and mobile games. The West is just catching up. This isn’t a lifestyle issue - it’s a civilizational collapse disguised as obesity.
Lorena Druetta
I was diagnosed with prediabetes last year. I started doing the DPP program through my employer. My coach was a retired nurse. We met weekly. I lost 18 pounds. My HbA1c is normal now. It’s not magic. It’s just showing up.
Roshan Gudhe
The body is not a machine. It’s a conversation. When you flood it with sugar, you’re not just breaking a dial - you’re shouting at a friend who’s trying to listen. The silence that follows isn’t indifference. It’s exhaustion. Healing begins when you stop screaming and start listening.
Jhoantan Moreira
I’ve been following this for years. The real tragedy isn’t the syndrome - it’s how we treat people who have it. Like they’re lazy or weak. I know someone who lost 50 lbs and still gets stared at in the grocery store. Compassion matters more than cholesterol numbers.
Caleb Sutton
This is all a Big Pharma scam. They don’t want you to heal. They want you on statins, metformin, and blood pressure pills forever. The real cause? Glyphosate in your food. And the CDC is covering it up.
Jesse Naidoo
I read this and immediately thought about my ex. She had all five markers. I told her she was going to die young. She left me. Now she’s doing yoga and eating kale. I guess I was right. But I miss her.
Justin Fauth
America’s got it easy. In my dad’s village in Texas, they still eat cornbread and lard. No one’s got time for ‘metabolic syndrome.’ They just work, eat, and pray. If God wants you alive, you’re alive. No app can fix that.
Joy Johnston
It is imperative to underscore that the efficacy of lifestyle interventions, as validated by the Diabetes Prevention Program, remains the gold standard in clinical practice. Pharmacological adjuncts, while beneficial, do not constitute a curative modality. Adherence to evidence-based behavioral protocols is non-negotiable.
Samuel Bradway
My mom had it. She started walking every morning. Cut out soda. Started cooking. Two years later, she’s off all meds. She says the best part? She can now play with her grandkids without getting winded. That’s the real win.