MAOI-Opioid Interaction Checker
Check Your Medication Safety
This tool checks if your medication is safe to take while on MAOIs. Dangerous interactions can cause life-threatening serotonin syndrome.
Critical Washout Period Guidance
When switching between MAOIs and opioids:
- Irreversible MAOIs (Nardil, Parnate, Marplan): Wait 14 days after stopping before starting any opioid
- Reversible MAOIs (moclobemide): Wait 24 hours (only under medical supervision)
- Transdermal selegiline patch: Still wait 14 days
DO NOT skip this washout period - it's a known cause of death
Combining opioids with MAOIs isn't just risky-it can kill you. This isn't theoretical. People have died from this mix, sometimes within hours of taking their first dose. And yet, doctors still prescribe it. Patients still take it. And too many don’t know they’re playing Russian roulette with their nervous system.
Why This Combination Is a Time Bomb
MAOIs-monoamine oxidase inhibitors-are antidepressants like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan). They work by blocking enzymes that break down serotonin, norepinephrine, and dopamine. That’s good for depression. But when you add certain opioids, you’re flooding your brain with even more of these chemicals. The result? Serotonin syndrome. Serotonin syndrome isn’t just anxiety or nausea. It’s a full-body meltdown: your temperature spikes above 104°F, your muscles lock up like concrete, you seize, your blood pressure rockets, and your organs start shutting down. A 2019 review found 2-12% of severe cases end in death. And it doesn’t take long. One patient on Reddit described his core temperature hitting 107.1°F after taking tramadol while on phenelzine. He spent three days in intensive care.The Opioids That Can Kill You
Not all opioids are equally dangerous. Some are outright banned with MAOIs. Others are ticking time bombs.- Meperidine (Demerol): The deadliest. Over 37 documented deaths since the 1960s. It doesn’t just raise serotonin-it releases it directly. The FDA calls it absolutely contraindicated. No exceptions.
- Tramadol: The most common offender. Prescribed as a "non-narcotic," it’s actually a weak opioid with strong serotonin reuptake inhibition. Over 68 cases of serotonin syndrome linked to MAOIs since 2010. One 2021 study found it caused more than half of all MAOI-opioid emergencies.
- Methadone: Used for pain and addiction, it blocks serotonin reuptake and also affects NMDA receptors. Dangerous enough that the FDA includes it in its black box warning.
- Dextromethorphan: Found in cough syrups. Even OTC versions can trigger this reaction. People don’t realize they’re taking an opioid-like drug.
- Tapentadol (Nucynta): Similar to tramadol. Purdue Pharma paid a $4.7 million settlement in 2021 for failing to warn about this interaction.
Even "Safe" Opioids Aren’t Risk-Free
Morphine, oxycodone, and hydromorphone are often called "safer"-and they are, relatively. But they still carry risk. They don’t directly release serotonin like meperidine, but they can still increase its levels indirectly. There are documented cases of serotonin syndrome with these drugs too, especially in older patients or those on high MAOI doses. And here’s the kicker: even reversible MAOIs like moclobemide aren’t safe. A 2017 study showed tramadol combined with moclobemide still caused serotonin syndrome at normal doses. The idea that "it’s just a mild MAOI" is dangerously wrong.
How Long Do You Have to Wait?
If you’re switching from an MAOI to an opioid-or vice versa-you can’t just stop one and start the other the next day. The enzymes your body needs to break down these drugs take time to recover.- For irreversible MAOIs (Nardil, Parnate, Marplan): Wait 14 days after stopping before starting any opioid with serotonergic activity.
- For reversible MAOIs (moclobemide): A 24-hour washout is usually enough-but only under strict medical supervision.
- For the transdermal selegiline patch: The FDA still recommends 14 days, even though it’s less brain-penetrating.
What Can You Use Instead?
If you’re on an MAOI and need pain relief, you have options-but you must be careful.- Buprenorphine: At low doses (0.2-0.4 mg sublingual), it’s been safely used in over 140 patients on MAOIs with no serotonin syndrome cases reported.
- Acetaminophen (Tylenol): Safe. No interaction. First-line for mild to moderate pain.
- NSAIDs: Ibuprofen, naproxen. Safe for most people, though watch for kidney or stomach issues.
- Physical therapy, nerve blocks, acupuncture: Non-drug options that work well for chronic pain.
Doctors Still Get This Wrong
You’d think this would be common knowledge by now. But it’s not. A 2022 study in JAMA Internal Medicine found that 4.3% of MAOI users got a contraindicated opioid within 14 days of starting the antidepressant. That’s over 11,000 dangerous prescriptions every year in the U.S. alone. Primary care doctors made 63% of these errors. Not psychiatrists. Not pain specialists. Regular family doctors who didn’t know the risk. Even worse: a 2022 survey in the Annals of Emergency Medicine found 31% of ER doctors didn’t know tramadol was contraindicated with MAOIs. That means if you show up in an emergency with severe pain, the person treating you might give you the exact drug that could kill you.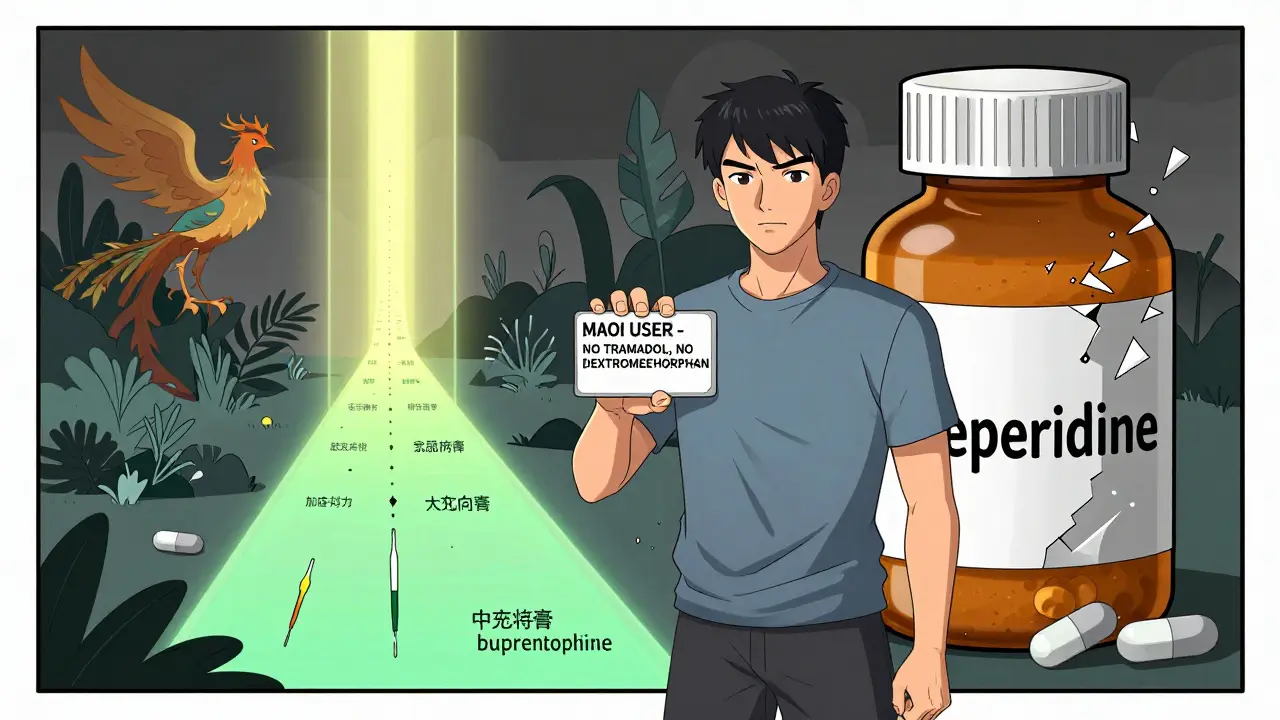
Technology Is Trying to Help
Thankfully, systems are catching up. Electronic health records like Epic now have hard stops-they won’t let a doctor prescribe tramadol to someone on Nardil. In 2021, they blocked over 8,400 dangerous prescriptions. But 1,200 of those were overridden. Why? Because the doctor didn’t know better-or thought, "This patient needs it, so I’ll just make an exception." There’s also a new digital tool called SerotoninSafe, approved by the FDA in 2023. It connects to hospital systems and gives real-time alerts. In a pilot at Johns Hopkins, it cut prescribing errors by 76%.What You Need to Do Right Now
If you’re on an MAOI:- Check every medication you take-even OTC cough syrup. Look for dextromethorphan, tramadol, or methadone.
- Carry a wallet card listing your MAOI and all contraindicated drugs. The National Alliance on Mental Illness provides them free. 78% of users carry theirs.
- Tell every doctor, dentist, and pharmacist you’re on an MAOI-even if they don’t ask.
- If you’re scheduled for surgery, tell the anesthesiologist. Meperidine is still used in some operating rooms.
- Never start or stop an MAOI without consulting your psychiatrist. The 14-day rule is non-negotiable.
- Know the signs of serotonin syndrome: fever, muscle rigidity, confusion, rapid heart rate, sweating, tremors.
- If someone on an MAOI takes an opioid and suddenly gets worse-call 911 immediately. Don’t wait.
- Keep cyproheptadine on hand if your loved one is at high risk. It’s an antidote, but it must be given early.
The Bottom Line
This isn’t a "maybe dangerous" situation. It’s a confirmed killer. Over 127 cases of serotonin syndrome linked to MAOI-opioid combinations have been reported since 2010. Nearly 90 people have died. The science is clear. The warnings are loud. The FDA, WHO, and every major medical society agree: do not combine these drugs. If you’ve been prescribed an opioid while on an MAOI, stop. Don’t wait. Call your doctor or pharmacist today. Ask: "Is this safe with my MAOI?" If they hesitate, walk out and find someone who knows the answer. Your life isn’t worth the risk.Can I take tramadol if I’m on an MAOI?
No. Tramadol and MAOIs together can cause serotonin syndrome, which can be fatal. Over 68 cases have been documented since 2010, and it’s one of the most common causes of emergency visits among MAOI users. Even if your doctor says it’s "low risk," the evidence shows it’s not worth the chance.
How long after stopping an MAOI can I take opioids?
Wait at least 14 days after stopping an irreversible MAOI like Nardil or Parnate before starting any opioid with serotonergic effects. For reversible MAOIs like moclobemide, 24 hours may be enough-but only under direct medical supervision. The 14-day rule exists because it takes that long for your body to rebuild the enzymes that break down excess serotonin.
What painkillers are safe with MAOIs?
Acetaminophen (Tylenol), ibuprofen, and naproxen are generally safe. Low-dose buprenorphine (0.2-0.4 mg) has been used safely in clinical studies. Avoid all opioids that affect serotonin: tramadol, methadone, meperidine, dextromethorphan, and tapentadol. Always confirm with your doctor or pharmacist before taking anything new.
Is it safe to take cough medicine with an MAOI?
Many over-the-counter cough syrups contain dextromethorphan, which is chemically similar to opioids and can trigger serotonin syndrome when combined with MAOIs. Always check the label. If it lists dextromethorphan, don’t take it. Use saline sprays, honey, or guaifenesin instead.
What should I do if I accidentally took an opioid while on an MAOI?
Seek emergency help immediately. Symptoms like high fever, muscle stiffness, confusion, or rapid heartbeat can develop within hours. Call 911 or go to the ER. Tell them you’re on an MAOI and took an opioid. Time is critical. Cyproheptadine, benzodiazepines, and cooling treatments can save your life if given early.
Why do doctors still prescribe opioids to MAOI users?
Many don’t know the risk. A 2022 study found 31% of emergency doctors didn’t know tramadol was contraindicated with MAOIs. Others assume the patient "must know," or think the pain is urgent enough to justify the risk. Electronic systems now block these prescriptions, but 14% are still overridden. This is a persistent educational gap that’s costing lives.


Ben Harris
So let me get this straight-your doctor gives you a drug that can turn your body into a human furnace and you just shrug and take it because 'it's just a cough syrup'? I've seen people die from this and no one talks about it like it's a fucking horror movie because everyone's too busy Googling 'natural pain relief' instead of reading the goddamn label
Jason Jasper
I’ve been on phenelzine for 8 years. Took tramadol once for a toothache back in 2019. Didn’t know any better. Ended up in the ER with 105°F fever and muscle spasms. They pumped me full of cyproheptadine. I’m alive but I still get nightmares about that night. Please, just check the labels. It’s not worth it.
Zabihullah Saleh
There’s something deeply tragic about how we treat medicine like a menu-pick what feels good, ignore the fine print, assume the system has your back. But here’s the thing: your body doesn’t care about your intentions. It only responds to chemistry. MAOIs + opioids = biological betrayal. No heroism in surviving it. No glory in the ICU. Just a broken nervous system and a lesson learned too late.
And yet, we keep doing it. Because we’re taught to trust doctors blindly. Because we’re told 'it’s just a little bit.' Because we’re scared of pain more than we’re scared of death. We need better education-not just warnings. We need culture change.
It’s not just about drugs. It’s about how we value life when it’s inconvenient to pay attention.
Winni Victor
Oh my god I’m so mad right now. Like, why is this even a thing? Who thought it was a good idea to put dextromethorphan in cough syrup and then not put a skull and crossbones on it? I swear if I find out some pharma exec made a PowerPoint slide saying 'Let’s see if people die from this' I’m gonna personally haunt their LinkedIn
Also I just checked my medicine cabinet and I have Robitussin. I’m throwing it out. And I’m telling my mom. And her dentist. And her yoga teacher. And her cat. The cat needs to know.
Lindsay Hensel
As a registered nurse with over 15 years in psychiatric and emergency care, I have witnessed firsthand the catastrophic consequences of this interaction. Serotonin syndrome is not a 'side effect'-it is a medical emergency that progresses with terrifying speed. The 14-day washout period is not arbitrary; it is a biological imperative. Please, for the love of all that is holy, verify every medication with your pharmacist. Do not rely on memory. Do not assume. Always confirm.
Christopher King
Did you know the FDA is just a puppet of Big Pharma? They knew about this for decades but let people die so they could keep selling opioids and antidepressants. The 14-day rule? A joke. They want you scared so you'll keep taking pills. They don't want you healed-they want you dependent. And now they've got AI systems blocking prescriptions like it's some kind of digital police state. Wake up. This isn't safety. It's control.
My cousin died from this. They said 'accidental overdose.' But I know. They didn't want to admit the truth. The system is rigged. And you're being lied to.
sagar patel
Tramadol is not an opioid. It is a serotonin-norepinephrine reuptake inhibitor with weak mu-opioid activity. This distinction matters. The literature is clear: the risk is dose-dependent and modulated by CYP2D6 metabolism. Not all MAOIs are equal. Moclobemide has reversible inhibition. The 14-day rule is conservative. Clinical judgment must prevail. Not fear.
Linda B.
Wow. So now we’re supposed to trust a 2022 study that says 31% of ER docs don’t know this? And you’re surprised? The same system that gave us Vioxx and OxyContin is now giving us 'SerotoninSafe' like it’s some kind of magic app? Please. If this were really a priority, they’d ban dextromethorphan over the counter. But they won’t. Because profit > people. Again.