For decades, oral corticosteroids (OCS) have been the go-to rescue for severe asthma flare-ups. They work fast. They save lives. But for many patients, that relief comes with a heavy price tag-on their body, their wallet, and their long-term health. If you or someone you know is on daily or frequent OCS for asthma, you’re not alone. But you also don’t have to stay stuck there. There are real, science-backed alternatives that can cut or even eliminate the need for these pills-without putting breathing at risk.
Why Oral Corticosteroids Are a Double-Edged Sword
Oral corticosteroids like prednisone and prednisolone are powerful anti-inflammatories. In an acute asthma attack, they can stop a hospital visit in its tracks. GINA guidelines recommend short courses of 3-5 days for kids and 5-7 days for adults during flare-ups. That’s fine. The problem isn’t occasional use. It’s dependence. When someone needs OCS for six months or longer, that’s not management-it’s a sign the asthma isn’t under control. And it’s far more common than many realize. One 2025 study found 93% of people with severe asthma suffered side effects directly tied to OCS use, even if they weren’t on it every day. These aren’t minor complaints. They include weight gain, type 2 diabetes, bone thinning (osteoporosis), eye pressure leading to glaucoma, mood disorders like anxiety and depression, heart problems, and even adrenal insufficiency-where the body stops making its own cortisol because it’s been flooded with synthetic versions for too long. And the damage doesn’t stop at symptoms. A 2025 study in Italy calculated that each asthma patient on long-term OCS adds nearly €1,960 a year in extra healthcare costs just from treating the side effects. That’s almost double what non-asthma patients pay for similar complications. Meanwhile, the pills themselves cost pennies. The real cost is hidden in ER visits, fractures, insulin prescriptions, and mental health care.Biologics: The Game-Changing Alternative
The biggest shift in severe asthma care over the last decade isn’t a new inhaler. It’s biologics. These are targeted, injectable or infused drugs that silence specific parts of the immune system driving inflammation in asthma. Unlike OCS, which blanket the whole body, biologics hit only the troublemakers. Six are approved for asthma right now: omalizumab, mepolizumab, reslizumab, benralizumab, dupilumab, and tezepelumab. They’re not for everyone. They work best in people with type 2 inflammation-a subtype found in about half to two-thirds of severe asthma cases. That’s measured through blood tests (eosinophils) or FeNO (fractional exhaled nitric oxide), both now standard in specialist clinics. The results speak for themselves. In a 2023 study of 106 Italian adults with uncontrolled asthma, mepolizumab slashed OCS dependence from 79% to just 31% in under a year. Daily steroid doses dropped by nearly 5 mg on average. Exacerbations fell from 4.1 per year to 0.8. Hospitalizations dropped from 4 in 10 patients to just 6%. Dupilumab showed similar results in multiple trials, cutting both flare-ups and OCS use by more than half. These aren’t just numbers. Patients report feeling like they’ve gotten their life back. Fewer missed workdays. Less fear of the next attack. No more bloating, insomnia, or mood swings from steroids. One woman in Nottingham, on biologics for 18 months, told her pulmonologist: “I didn’t realize how tired I was until I wasn’t taking prednisone every other month.”
Why Aren’t More People on Biologics?
If they’re this effective, why aren’t they first-line treatment? Two big reasons: access and cost. Biologics cost thousands per year. OCS cost less than £10 for a month’s supply. On paper, OCS win. But that ignores the hidden costs-the hospital stays, the bone scans, the diabetes meds, the mental health support. When you add it all up, studies show biologics actually save money over time. The Italian data proved it: fewer hospital visits meant lower overall spending, even with the drug price tag. The bigger barrier? Getting tested and referred. Not every GP knows how to identify type 2 asthma. Not every clinic has the lab access or the specialist slots. And insurance coverage varies wildly. In the UK, NHS access to biologics has improved but still depends on local commissioning and strict criteria. Patients often need to fail multiple controller therapies first. GINA guidelines now say: if you’re on maintenance OCS (even just 7.5 mg/day or less), you should be offered a biologic before staying on steroids long-term. That’s a major shift. But in practice, many patients are still being kept on OCS because the system hasn’t caught up.Other Options-What Works, What Doesn’t
Beyond biologics, there are other paths, but they’re either narrow or unproven. Bronchial thermoplasty is a procedure where a catheter delivers heat to the airway muscles, reducing their ability to tighten during an attack. It’s done in three sessions under sedation. Studies show it can reduce exacerbations and improve quality of life-but only for a small group: severe asthma patients who’ve tried everything else. And in the six weeks after treatment, symptoms often get worse before they get better. It’s not a first choice. It’s a last resort. What about vitamins? Many patients try vitamin D, hoping it’ll help. But multiple trials, including a 2021 review by the American Academy of Family Physicians, found no benefit. High-dose vitamin D3 didn’t reduce flare-ups, didn’t improve lung function, and didn’t cut steroid use in adults with asthma-even those who were deficient. Lifestyle changes matter. Quitting smoking, losing weight if overweight, managing stress-all help. But they don’t replace the need for targeted medical therapy in severe cases. They’re support, not substitutes.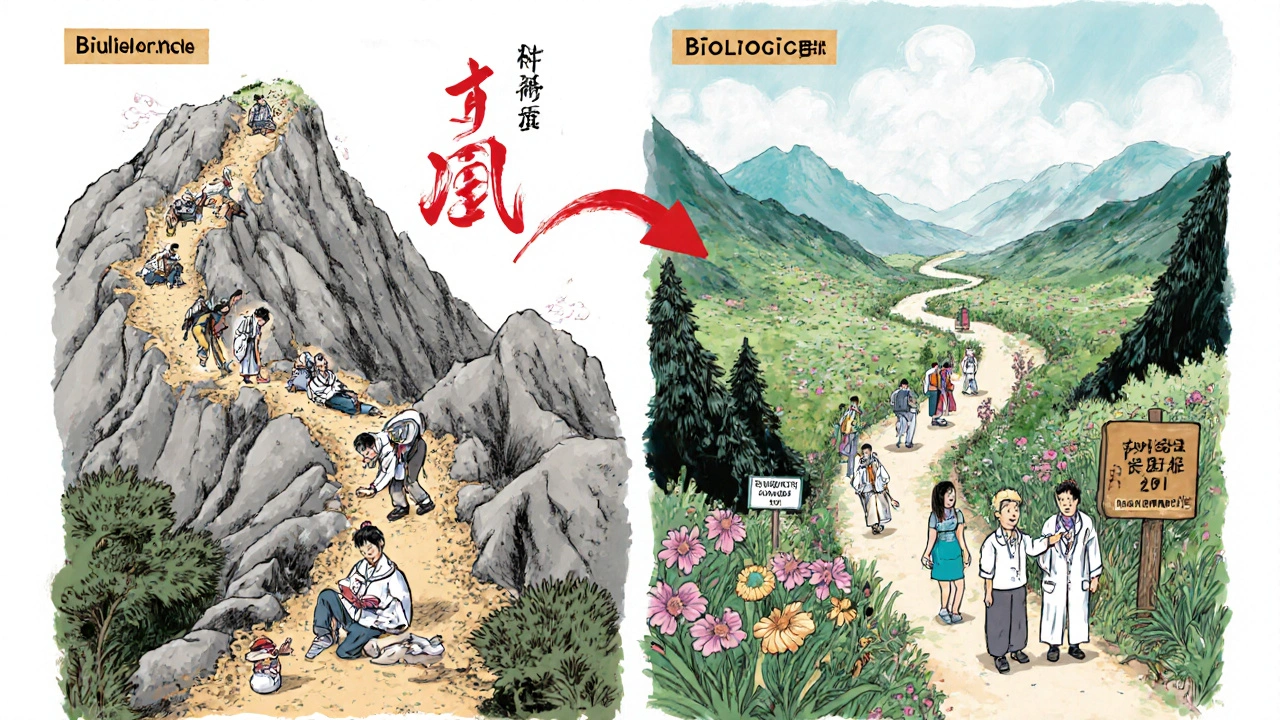
How to Start the Transition
If you’re on long-term OCS and want out, here’s how to begin:- Get tested for type 2 inflammation. Ask for a blood eosinophil count and FeNO test. These are simple, non-invasive, and covered by most insurers.
- Review your asthma control. Are you on the right inhaled corticosteroid dose? Are you using a spacer? Are you taking your meds correctly? Poor technique can make asthma seem worse than it is.
- Talk to your respiratory specialist about biologics. Don’t wait for them to bring it up. Bring the data: “I’ve been on prednisone for 8 months. What are my options to get off it?”
- Ask about a steroid taper plan. You can’t stop OCS cold turkey. Your body needs time to restart its own cortisol production. A slow, monitored reduction-over weeks or months-is essential.
- Track your symptoms. Use a peak flow meter and asthma diary. Note how you feel before, during, and after starting a biologic. This helps your team adjust safely.
The Bigger Picture: Changing the Rules
The medical world is finally waking up to the fact that OCS are not a long-term solution. They’re a Band-Aid on a broken system. The goal isn’t to manage side effects-it’s to fix the asthma so you don’t need them at all. The 2023 Advances in Therapy ‘Charter’ called for a fundamental reset: move biologics earlier in the treatment ladder, not at the very end. That’s happening slowly. In some UK centers, patients now get biologic referrals after just one hospital admission for asthma, not after years of OCS. The economic case is clear. The clinical case is clear. The patient experience is clear. The only thing holding us back is inertia-and access. If you’re on daily or frequent oral steroids for asthma, you’re not failing. The system is. But change is here. And you have more power than you think to ask for it.Can I stop taking oral corticosteroids on my own?
No. Stopping oral corticosteroids suddenly can cause adrenal crisis, a life-threatening condition where your body can’t make enough cortisol. Always work with your doctor on a slow, monitored taper plan-usually over weeks or months-especially if you’ve been on them for more than a few weeks.
Are biologics safe for long-term use?
Yes. Biologics have been used for over a decade in asthma, and long-term safety data is strong. The most common side effects are mild: injection site reactions, headaches, or sore throat. Serious infections are rare and occur at rates similar to placebo in clinical trials. They don’t cause weight gain, diabetes, or bone loss like oral steroids do.
How do I know if I have type 2 inflammation?
Your doctor can test for it with two simple checks: a blood test for eosinophils (a type of white blood cell linked to allergic inflammation) and a FeNO test, where you breathe into a device that measures nitric oxide in your breath. High levels of either suggest type 2 asthma, which responds best to biologics.
Do biologics cure asthma?
No. Biologics don’t cure asthma, but they can dramatically reduce how often you flare up and how much you rely on steroids. Many patients reach a point where they’re asthma-free for months at a time. It’s not a cure, but it’s the closest thing we have to normal life with severe asthma.
Is there financial help for biologics in the UK?
Yes. In England and Wales, biologics are available through NHS specialist asthma clinics if you meet strict clinical criteria. Some patients may qualify for patient assistance programs offered by drug manufacturers. Ask your respiratory nurse or pharmacist-they often know about funding routes that aren’t widely advertised.


Dana Dolan
Wow. I’ve been on prednisone for 3 years and didn’t realize how much it was stealing from me - my sleep, my mood, my waistline. Just found out I’m type 2 inflamed. Scheduled my eosinophil test tomorrow. Feels like a lifeline.
Zac Gray
Let’s be real - biologics are the future, but the system is still stuck in the 1990s. My doc said ‘try this for six months’ and handed me a 30-day script of prednisone. Meanwhile, the biologic cost is more than my rent. And no, insurance won’t cover it until I’ve been hospitalized twice. Classic.
seamus moginie
This article is a masterpiece. The data is irrefutable. We are wasting lives and billions on outdated protocols. If you’re on OCS long-term, you’re not being treated - you’re being tolerated. It’s time to demand better. Biologics aren’t optional. They’re essential. And if your doctor doesn’t know that, find a new one.
Michael Salmon
Biologics? More like bioweapons. Big Pharma’s way of locking people into lifelong injections while they charge $50K a year. You think this is medicine? It’s a cash grab dressed up as science. OCS are cheap. They’re nasty. But at least you know what you’re getting. These biologics? They’re black boxes with price tags.
Steve and Charlie Maidment
So let me get this straight - you’re telling me that instead of taking a $5 pill every other day, I should pay $40,000 a year for a shot? And you call that progress? My cousin took one of those ‘biologics’ and got shingles. So now we’re trading steroid weight gain for viral infections? Thanks, science.
Ellen Calnan
I stopped prednisone last year after 7 years. It took 14 months to taper. I cried the first week I didn’t feel like a zombie. I didn’t realize how much my brain had been fogged by cortisol. Now I can think. I can laugh. I can sleep through the night. Biologics didn’t cure me - but they gave me back my soul. And that’s worth every penny.
Derron Vanderpoel
Just got my FeNO results - 42 ppb. My pulmonologist said ‘you’re textbook type 2.’ I cried. Not from sadness - from relief. For years I thought I was just ‘bad at asthma.’ Turns out my body was screaming for help - and no one was listening. Biologic appointment booked. This feels like the first real step forward.
Michael Petesch
As someone who has studied global asthma management protocols, I find it remarkable how disparate access remains. In the U.S., cost barriers are systemic. In the U.K., bureaucratic gatekeeping delays care. In India, biologics are nearly inaccessible. Yet the clinical evidence is universal. This is not a medical failure - it is a policy failure.
Reema Al-Zaheri
I have severe asthma. I am from India. I have never heard of FeNO testing. My inhaler costs $2. Prednisone costs $1. Biologics? Unthinkable. I am grateful for this information - but it feels like a luxury for people in rich countries. How do we make this accessible globally?
Joe Durham
Reading all this, I feel so much for people stuck on OCS. I used to think ‘just take the pill, it’s easier.’ But now I see - it’s not easier. It’s a slow erosion. The fact that patients have to fight just to get tested… that’s the real tragedy. We need to change how we think about asthma care. It’s not about compliance - it’s about justice.
Angela Gutschwager
Biologics = scam. OCS = evil. What’s the middle ground? 😒
Andrew Baggley
You don’t need to wait for your doctor to bring it up. Print this article. Highlight the GINA guidelines. Walk into your appointment and say, ‘I’m done with prednisone. What’s my next step?’ Most docs are overwhelmed - they need you to lead. You’re not being difficult. You’re being smart.
Codie Wagers
Let’s be honest - this isn’t about asthma. It’s about control. The medical industrial complex needs you dependent. OCS? Easy to prescribe. Biologics? Require coordination, labs, specialists. That’s too much work. So they keep you on the pill. And you call it ‘care.’ It’s exploitation dressed in white coats.
Sam Reicks
They say biologics are safe but what about the 2021 CDC memo that linked them to mysterious neurological cases in 12 states? No one talks about it. And why? Because the FDA is owned by Big Pharma. I’ve been on prednisone for 10 years. At least I know what’s in it. Glyphosate? Nope. Just cortisol. I’ll take my chances.
Timothy Reed
This is exactly the conversation we need more of. I’m a respiratory nurse. I’ve watched patients deteriorate on OCS because no one pushed the alternative. I’ve seen the relief on faces when biologics finally kick in. It’s not magic. It’s medicine. And it’s time we stop treating it like a last resort. Start the conversation early. Test early. Act early.