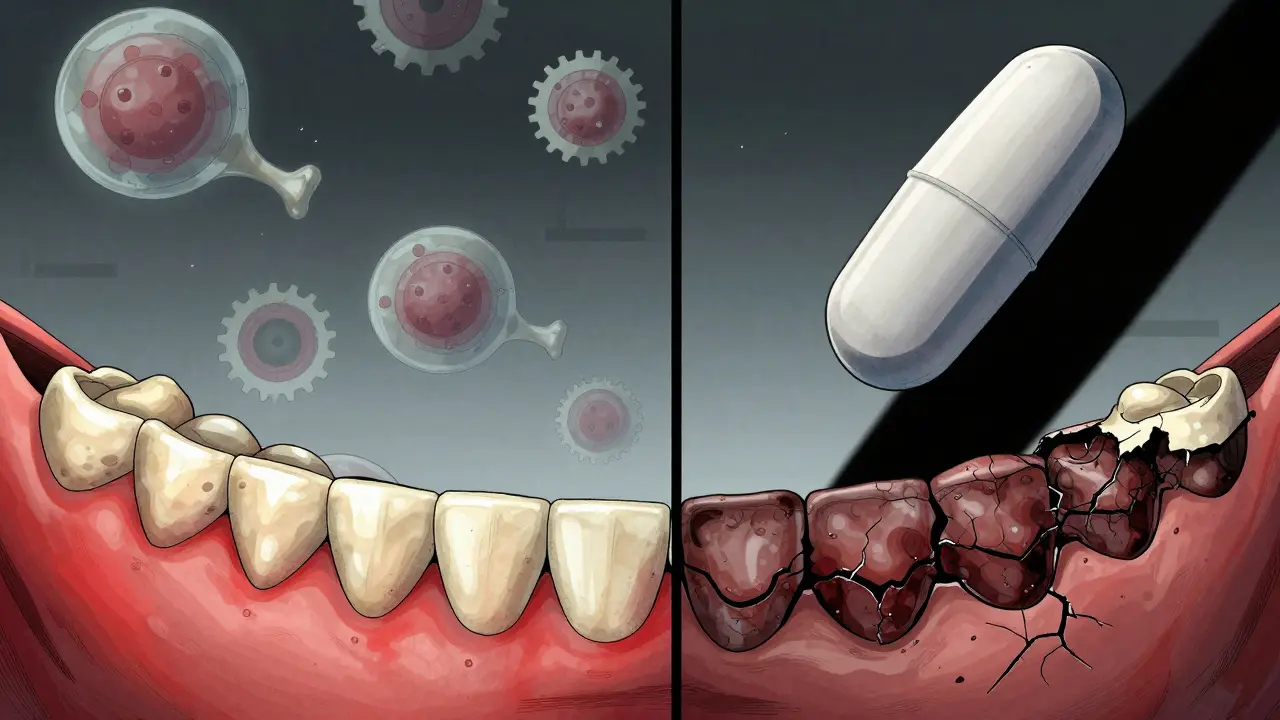
When you’re diagnosed with osteoporosis, your doctor’s main goal is simple: prevent broken bones. That’s why medications like bisphosphonates are so widely prescribed. They’re effective, affordable, and backed by decades of research showing they can cut hip and spine fracture risk by up to 70%. But for every benefit, there’s a shadow - and for some people, that shadow is a rare but serious condition called medication-related osteonecrosis of the jaw, or MRONJ.
What Exactly Is MRONJ?
MRONJ isn’t just a sore tooth or a minor infection. It’s when bone in your jaw becomes exposed and doesn’t heal for more than eight weeks. You might see it as a piece of bone sticking out near a pulled tooth, or feel persistent pain and swelling in your gums. It doesn’t happen overnight. It often shows up months or even years after a dental procedure - like an extraction - and it’s almost always linked to drugs that slow down bone breakdown.
The name used to be BRONJ - bisphosphonate-related osteonecrosis of the jaw. But now we know other drugs, like denosumab (Prolia), can cause it too. So the updated term is MRONJ: medication-related osteonecrosis of the jaw. The key trigger? Drugs that stop osteoclasts - the cells that naturally remove old bone so new bone can grow. Without that turnover, your jawbone can’t repair itself after trauma or infection.
Why the Jaw? It’s Not Just Any Bone
Why does this happen in the jaw and not the hip or spine? It comes down to biology. The bone in your jaw - especially the alveolar bone that holds your teeth - turns over about ten times faster than the bone in your leg or spine. That means it absorbs more of the medication. Add to that the constant presence of bacteria from your mouth, the stress of chewing, and thin gum tissue that’s easy to damage, and you’ve got a perfect storm.
Think of it this way: your leg bone doesn’t get brushed twice a day or chew on hard food. Your jaw does. And if the bone can’t heal because the drugs have shut down its repair system, even a small cut or infection can turn into something serious.
How Common Is It Really?
Here’s the truth most patients don’t hear: for someone taking oral bisphosphonates like alendronate (Fosamax) or risedronate (Actonel) for osteoporosis, the risk is incredibly low. Studies show about 0.7 cases per 100,000 people per year. That’s less than one in a hundred thousand. For context, you’re far more likely to be struck by lightning than develop MRONJ from these pills.
But the numbers change dramatically with intravenous (IV) drugs. Zoledronic acid (Reclast), given once a year for osteoporosis, carries a risk of about 1 in 100,000 per year. That’s still rare - but it’s 14 times higher than oral versions. And if you’re getting high-dose IV bisphosphonates for cancer, the risk jumps to 3% or more.
Denosumab (Prolia), a newer osteoporosis drug, may carry a slightly higher risk than oral bisphosphonates - about 1.7 to 2.5 times higher. But even then, the absolute risk remains very low. A 2024 study of 260,000 osteoporosis patients found no increased risk of jaw necrosis in those taking oral bisphosphonates compared to those not taking them at all.
The Real Culprit: Dental Work and Poor Oral Health
Most cases of MRONJ in osteoporosis patients happen after a dental extraction. In fact, 63% of cases reported to the American Association of Oral and Maxillofacial Surgeons followed a tooth removal. The median time from surgery to diagnosis? Just over two years.
But here’s the critical point: if you have gum disease, loose teeth, or untreated infections before starting bisphosphonates, your risk goes up. That’s why experts say the best way to prevent MRONJ is to get your mouth healthy before you start the medication. A full dental exam, cleaning, and any needed extractions or fillings should happen before you take your first pill.
Dr. Cesar Migliorati, who helped first identify this link in 2003, puts it bluntly: “If a lot of patients had gum disease or tooth infection before starting treatment, that could have raised the rate of ONJ.”
Drug Holidays: A Risky Balancing Act
Some doctors consider a “drug holiday” - stopping the medication for a few months before major dental work - to lower MRONJ risk. But this isn’t simple. Bisphosphonates stay in your bones for years, even after you stop taking them. A 2024 study in Nature Communications found that stopping IV zoledronic acid for more than 365 days reduced MRONJ risk by 82%. But it also increased the risk of a new fracture by 28%.
That’s the tightrope walk. Stopping the drug to protect your jaw might put your spine or hip at risk. For most people on oral bisphosphonates, the advice is simple: don’t stop without talking to your doctor. The fracture risk is real. The jaw risk? Still extremely low.
What Should You Do If You’re on Bisphosphonates?
- Before starting: Get a full dental checkup. Fix cavities, treat gum disease, and remove problem teeth. Don’t delay.
- While taking it: Brush and floss daily. See your dentist every six months. Tell them you’re on a bisphosphonate. Avoid invasive procedures if possible - but don’t refuse needed care out of fear.
- If you need an extraction: Work with both your doctor and dentist. They can coordinate care. In most cases, extraction is safe if your mouth is healthy and you’re on oral meds.
- Don’t panic: If you notice exposed bone, pain, or swelling after dental work, see your dentist immediately. Early treatment works better.
What About Denosumab?
Denosumab (Prolia) works differently than bisphosphonates. Instead of sticking to bone for years, it’s a monthly or biannual injection that blocks a protein called RANKL. It’s just as good at preventing fractures - but it clears from your body faster. That means if you stop taking it, your bone density can drop quickly. That’s why you can’t just quit it cold turkey.
And yes, it carries a slightly higher MRONJ risk than oral bisphosphonates. But again - the absolute risk is still very low. A 2024 study of breast cancer patients found that switching from bisphosphonates to denosumab increased ONJ risk to 16%. But that was in cancer patients getting much higher doses. For osteoporosis patients, the risk remains under 1%.
What’s the Bottom Line?
The fear of jaw necrosis is real. Many patients worry about it more than they worry about breaking a hip. And that’s understandable. But the data doesn’t lie: for people with osteoporosis, the benefits of bisphosphonates far outweigh the risks.
You’re more likely to die from a hip fracture than from MRONJ. A 10-year study showed that taking alendronate reduces hip fracture risk by 55%. That’s life-changing. And for most people, the chance of developing MRONJ is less than 1 in 10,000.
That’s why major medical groups - the American Dental Association, the American Association of Oral and Maxillofacial Surgeons, and the National Osteoporosis Foundation - all agree: don’t avoid treatment because of fear. Do your part: keep your mouth healthy, tell your dentist you’re on these meds, and don’t skip your annual checkups.
What’s Changing in 2025?
Research is moving fast. The 2024 study on drug holidays is already changing how doctors think. The ADA is updating its guidelines for 2025 to include new data on how long you should wait after stopping IV bisphosphonates before dental surgery.
Future tools may help too. Doctors are testing urine tests that measure bone turnover markers - like NTX - to find out who’s at highest risk for MRONJ. The goal? Personalized treatment. Someone with low bone turnover and perfect oral health might stay on bisphosphonates for 10 years. Someone with gum disease and high turnover might switch to a different drug after 3-5 years.
For now, the message stays simple: treat your osteoporosis. Protect your teeth. Talk to your team. And don’t let fear keep you from living without fear of breaking a bone.
Can bisphosphonates cause jaw necrosis even if I never had dental work?
Yes, but it’s extremely rare. Most cases of MRONJ happen after a dental procedure like an extraction, especially if there’s existing infection or gum disease. However, there are documented cases where bone became exposed without a clear trigger - often in patients on long-term IV bisphosphonates. For oral bisphosphonate users, spontaneous MRONJ without dental trauma is almost unheard of.
Is it safe to get dental implants if I’m on bisphosphonates?
It depends. For patients on oral bisphosphonates for osteoporosis, dental implants are generally considered safe - especially if your oral health is good and you’ve been on the medication for less than three years. Many dentists will proceed with implants if you’re on alendronate or risedronate. But for those on IV bisphosphonates or who’ve been on oral meds for more than five years, the risk increases. Always get a full dental evaluation and discuss your medication history with both your dentist and prescribing doctor before proceeding.
How long do bisphosphonates stay in my bones?
Bisphosphonates bind tightly to bone and can remain there for years - sometimes over a decade. Even after you stop taking the pill, the drug slowly releases from your skeleton. That’s why the risk of MRONJ can persist long after you’ve discontinued treatment. This is why it’s so important to get your dental work done before starting the medication, or at least early in your treatment.
Should I stop taking my bisphosphonate before a tooth extraction?
For most people taking oral bisphosphonates for osteoporosis, the answer is no. Stopping the drug doesn’t significantly lower your risk of MRONJ, and it increases your chance of a fracture. For those on IV bisphosphonates (like zoledronic acid) who’ve been on treatment for 3-4 years, some doctors may recommend a 3-month to 1-year drug holiday before major surgery - but only if your fracture risk is low. Never stop your medication without consulting both your doctor and dentist.
What are the early signs of jaw necrosis?
Early signs include exposed bone in the mouth that doesn’t heal within 8 weeks, persistent pain or swelling in the jaw, numbness or heaviness in the jaw, and loosening of teeth without obvious cause. In stage 1, you may have no symptoms at all - just exposed bone. Stage 2 includes pain and infection. Stage 3 involves fractures or holes connecting the jaw to the skin. If you notice any of these, see your dentist immediately. Early detection improves outcomes.


Raushan Richardson
My grandma’s on Fosamax and she’s got the healthiest teeth in her retirement home. She brushes twice, flosses like it’s a religion, and sees her dentist every six months. No drama. No fear. Just smart habits. This whole MRONJ thing is scary on paper, but if you take care of your mouth, you’re basically playing it safe. Don’t let fear stop you from living.
Also, I work in a dental office - we’ve seen zero cases in osteo patients on oral meds. Zero. It’s like worrying about being hit by lightning while staying indoors.
dean du plessis
Been on alendronate for 4 years. Had a tooth pulled last year. No issues. Dentist knew I was on it. We did it slow, no drama. My jaw’s fine. My hips are stronger. I’d rather have a solid spine than a perfect jaw.
Life’s about trade-offs. This one’s worth it.
Jane Lucas
i just got my first pilla last week and my dentist said dont worry unless u got rotten teeth or plan on gettin em pulled. i got 2 cavities but they fixed em. im just gonna brush and chill. no panic. no drama. my bones need this more than my jaw needs to be perfect.
Gerald Tardif
It’s funny how we treat numbers differently depending on who’s saying them. 1 in 100,000 sounds tiny until it’s your jaw. But then again, 1 in 2 for a hip fracture? That’s not a number - that’s a life sentence. The real risk isn’t the drug. It’s ignoring your mouth. Or worse - ignoring your bones.
Get checked. Get fixed. Stay on track. That’s the playbook.
Miriam Piro
They told you it’s rare. But what if it’s being covered up? The pharmaceutical companies don’t want you to know how long bisphosphonates stick around - 10+ years. That’s not medicine. That’s a slow poison locked in your skeleton.
And why is it always the jaw? Coincidence? Or is it because the jaw is the weakest link in a system designed to keep you dependent? Think about it. Dentists are paid to do procedures. Doctors are paid to prescribe. Who benefits when you need a root canal after 5 years? Not you.
They want you scared of fractures so you stay on the drug. But what if your body’s trying to tell you something? What if your bones don’t need to be frozen? What if movement, sunlight, and real food could’ve done the same thing?
I’m not saying don’t treat osteoporosis. I’m saying don’t trust the system. Ask harder questions. Look beyond the pamphlets.
And yes - I’ve read the studies. And I still don’t trust them.
Kishor Raibole
It is with profound gravity that I must elucidate the systemic fallacy inherent in the current paradigm of pharmacological intervention for osteoporosis. The medical establishment, in its infinite wisdom, has reduced a complex physiological phenomenon - namely, the dynamic equilibrium of bone remodeling - to a binary equation: take drug, prevent fracture. This reductionism is not merely inadequate; it is morally perilous.
One must interrogate the epistemological foundations upon which the 70% fracture reduction statistic is predicated. Is it derived from randomized controlled trials with adequate follow-up? Or is it extrapolated from surrogate endpoints in populations with comorbidities? The data, while statistically significant, remains epistemologically fragile.
Moreover, the notion that MRONJ is ‘rare’ is a semantic sleight of hand. Rare for whom? For the healthy, the compliant, the dentally pristine? But what of the elderly, the diabetic, the immunocompromised? The marginalized? The statistics do not speak to them. They speak to the ideal patient - a myth.
And let us not forget the financial architecture of this edifice: the pharmaceutical-industrial complex, with its lobbying arms and continuing medical education sponsorships, has normalized this paradigm. The drug holiday? A corporate compromise. Not a medical breakthrough.
Therefore, I implore you: do not merely follow guidelines. Question the very architecture of care. Seek holistic alternatives. Consider nutrition. Consider biomechanics. Consider the wisdom of ancestral practices. For in the silence between the pills, perhaps lies the true path to skeletal integrity.
Chris Garcia
Let me tell you something about fear - it’s the only thing more contagious than a bad tooth. We’ve turned a medical tool into a monster because we’re scared of dying. But here’s the truth: we’re not scared of osteoporosis. We’re scared of losing control. Of being broken. Of becoming a burden.
So we fixate on the jaw. A visible wound. Something we can see. Something we can blame. Meanwhile, the silent fracture in the spine? The collapse no one talks about until you can’t stand up? That’s the real enemy.
I come from Lagos. We don’t have MRI machines in every village. We don’t have Fosamax on every shelf. But we know this: if you can walk, you live. If you can’t walk, you die. And I’ve seen grandmothers in village huts carry water on their heads at 75 because their bones held. Not because of pills. Because of movement. Because of community. Because they never stopped living.
So yes - take the pill if you need it. But don’t let it make you a prisoner. Move. Eat real food. Talk to your dentist. Don’t wait for a crisis. And if you’re scared? Be scared - but don’t let it be the loudest voice in the room.
Elizabeth Alvarez
They say it's rare... but what if they're lying? I read a whistleblower report from a former Pfizer scientist - they knew about the jaw necrosis cases early, but buried the data because the profit margins were too good. The FDA doesn't regulate these drugs like they do for cancer meds, even though the mechanism is the same. And why? Because osteoporosis affects old people. And old people don't vote. Or complain loudly enough.
And the 'drug holiday'? That's just a PR move. The drug stays in your bones for life. So if you get an extraction 10 years later? Too bad. You're still at risk. They just want you to think it's safe if you stop. It's not.
Also - have you ever noticed how every study says 'no increased risk' but never says 'zero risk'? That's not science. That's spin.
And don't even get me started on denosumab. It's just a more expensive version with the same hidden agenda. They're selling you a slow death in exchange for a few extra years of walking. I'd rather die fast than rot from the inside out.
They're testing urine tests now? That's just to make you feel like you're being 'personalized' while they keep selling you the same poison. Wake up.
I'm not anti-medicine. I'm pro-truth. And the truth is - they don't care if you lose your jaw. They care if you keep buying the pills.