When your heart arteries are clogged, you have two main options: PCI or CABG
If you’ve been told you need a procedure to reopen blocked heart arteries, you’ve probably heard the terms PCI and CABG. They’re both ways to restore blood flow to your heart, but they’re nothing alike. One is a quick catheter procedure. The other is open-heart surgery. Choosing between them isn’t about which is "better"-it’s about which is right for you.
Every year, hundreds of thousands of people in the U.S. get one of these two procedures. About 600,000 get a stent (PCI). Around 300,000 get bypass surgery (CABG). That’s not because one is more popular-it’s because doctors pick the tool that fits the job. And the job isn’t just about opening a clog. It’s about how long the fix lasts, how it affects your life, and whether it keeps you alive longer.
What is PCI? A stent through a tiny needle
PCI stands for Percutaneous Coronary Intervention. Most people just call it a stent procedure. Here’s how it works: A doctor threads a thin tube through an artery in your wrist or groin, up to your heart. Using X-ray guidance, they guide a tiny balloon to the blockage, pop it open, and slip in a metal mesh tube-a stent-to hold the artery open. Modern stents are coated with medicine to prevent re-clogging. This isn’t surgery. No cutting. No opening your chest.
The whole thing usually takes one to two hours. Most people go home the next day. You’re back to light activities in a few days. Many are back at work within a week. It’s no wonder it’s the go-to for many patients.
But here’s the catch: stents don’t last forever. About 5 to 10% of people need another procedure within five years because the artery narrows again. That number was 20 to 30% with older bare-metal stents. Drug-coated stents helped, but they’re still not a permanent fix for complex blockages.
What is CABG? Open-heart bypass surgery
CABG-Coronary Artery Bypass Grafting-is what most people think of as "bypass surgery." The surgeon takes a healthy blood vessel from your leg, arm, or chest and sews it around the blocked artery. Think of it like building a detour around a traffic jam. The most common and durable graft comes from the left internal mammary artery, connected directly to the main front artery of the heart (LAD). This graft has an 85 to 90% chance of staying open 10 years later.
This is major surgery. You’re on a heart-lung machine. Your chest is opened. The procedure takes three to six hours. You’ll be in the hospital for five to seven days. Recovery takes six to eight weeks. You’ll feel sore for months. Your sternum takes time to heal. Some people report brain fog or memory issues for a few weeks, though most clear up by the one-year mark.
But here’s what makes CABG powerful: it’s built to last. If you have multiple blockages, especially in the left main artery or the front descending artery, CABG gives you a much better shot at staying symptom-free for years. And for certain groups-like people with diabetes-it actually saves lives.
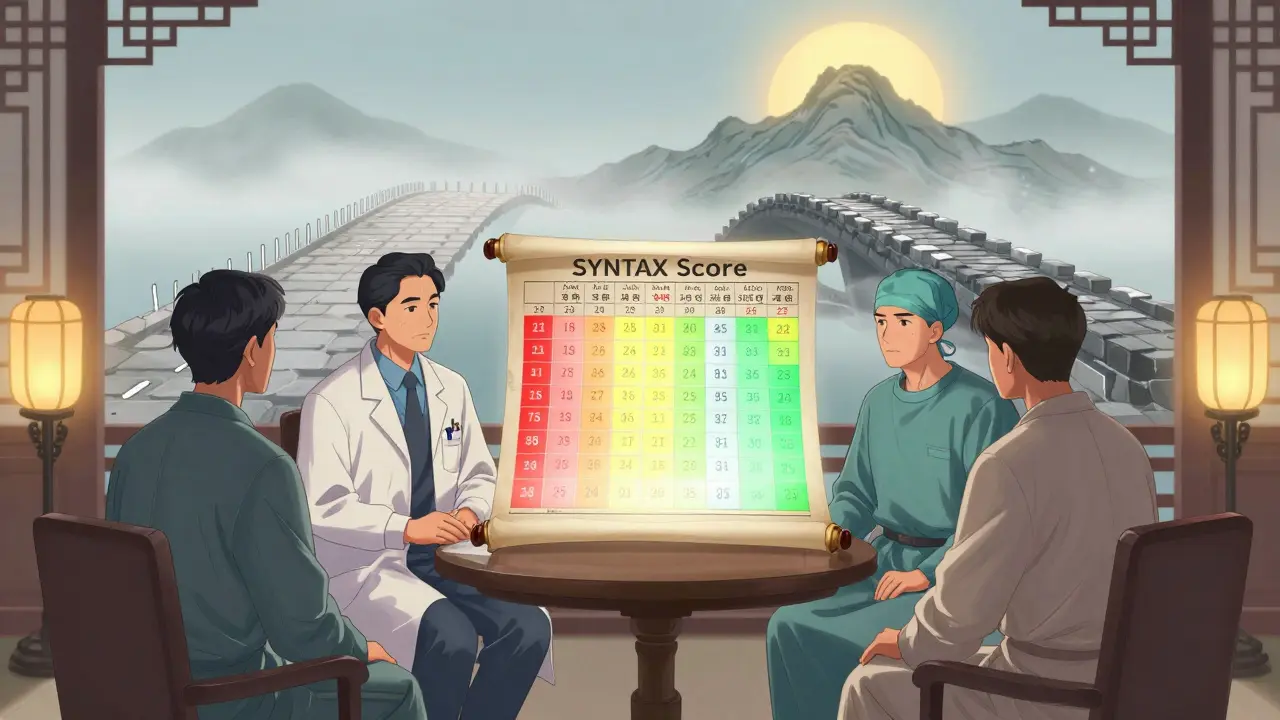
The SYNTAX Score: Your arteries’ complexity decides your path
Doctors don’t pick PCI or CABG based on gut feeling. They use a tool called the SYNTAX Score. It’s a detailed map of your coronary arteries, rated by how many blockages you have, where they are, and how bad they are. The higher the score, the more complex your disease.
- Score under 22: PCI is usually the better choice. Simple blockages respond well to stents.
- Score 22 to 32: This is the gray zone. Your heart team will weigh your age, diabetes, heart function, and preferences.
- Score over 32: CABG is strongly recommended. Complex disease means you need a durable fix.
This score isn’t just a number-it’s backed by massive studies. The SYNTAX trial showed that for patients with scores above 32, CABG cut major heart events by nearly 35% compared to PCI over five years. And the reason? Far fewer repeat procedures. People who got stents needed another intervention twice as often.
Diabetes changes everything
If you have diabetes and multi-vessel disease, the choice becomes clearer-and more urgent. The FREEDOM trial, one of the most important studies in heart care, followed 1,900 diabetic patients for five years. Those who got PCI had a 16.4% chance of dying. Those who got CABG? Only 10%.
That’s a 44% lower risk of death. Why? Because diabetes causes more widespread, diffuse artery damage. Stents work well on single blockages, but they struggle with the kind of widespread disease diabetes creates. CABG, with its durable grafts, is better equipped to handle it.
Guidelines now say CABG is the preferred option for diabetics with multi-vessel disease. It’s not a suggestion-it’s a Class IA recommendation, the strongest level of evidence.
Left main disease: The high-stakes decision
When the main artery feeding the left side of your heart is blocked, it’s dangerous. The EXCEL and NOBLE trials looked at this exact group. At first glance, PCI and CABG seemed similar. But the longer you look, the more the story changes.
At 30 days, PCI had a slight edge-fewer strokes, faster recovery. But after one year, the tide turned. By five years, CABG had a clear advantage: fewer heart attacks, fewer repeat procedures, and better long-term survival. The 5-year data showed CABG reduced the risk of death or heart attack by 39% compared to PCI in left main disease.
So if you have left main disease, especially with other risk factors, CABG isn’t just an option-it’s often the smarter long-term play.
Recovery: Fast and easy vs. slow and steady
Let’s talk about real life. After PCI, you might be back to walking your dog in two days. You can drive again in a week. Most people are back to work in under two weeks.
After CABG, it’s different. You’ll be in pain for weeks. Your chest feels tight. You can’t lift anything heavy. You need help getting dressed. It takes six to eight weeks to feel like yourself again. But here’s what patients say: once you get past the recovery, the relief is deeper.
A study called ROSETTA found that one year after surgery, 92% of CABG patients were completely free of chest pain. Only 85% of PCI patients said the same. And while 78% of PCI patients felt normal at 30 days, only 52% of CABG patients did. But by six months, nearly everyone in both groups was back to work.
It’s not about speed-it’s about sustainability. One is a quick fix. The other is a long-term reset.
The heart team: Why you need more than one doctor’s opinion
Guidelines now say your treatment decision must come from a heart team. That means an interventional cardiologist (who does stents) and a cardiac surgeon (who does bypass) sit down together-with you-and review your case.
This isn’t bureaucracy. It’s protection. A stent specialist might lean toward PCI. A surgeon might lean toward CABG. But when they talk to each other, they see the full picture. They check your SYNTAX score, your diabetes status, your kidney function, your age, your lifestyle. They look at your goals: Do you want to get back to work fast? Or do you want to avoid another procedure in five years?
High-volume centers-those doing over 400 PCIs or 200 CABGs a year-have better outcomes. That’s why it matters where you go. If your hospital doesn’t have a heart team, ask for a referral.
What about new tech? Are stents getting better? Is bypass changing?
Yes. Both sides are evolving.
Stent technology keeps improving. Newer drug coatings, thinner metal, and bioresorbable scaffolds (still in trials) promise fewer repeat procedures. But nothing has matched the durability of an arterial graft yet.
On the surgical side, surgeons are using more arterial grafts-like from the arm or chest-instead of veins from the leg. Early data shows this can boost 10-year survival from 74% to 82%. Robotic-assisted bypass is also emerging, reducing chest incisions and speeding recovery.
And there’s talk of "hybrid" procedures: a surgeon does a bypass on the front artery (LAD), and a cardiologist stents the other blockages. This could be the future for some patients. But it’s still experimental and only done in a few centers.
What do patients really say?
Online forums like Reddit are full of real stories. One user, u/CABGsurvivor, wrote: "Six weeks of recovery was tough, but two years later, I’m hiking again with no chest pain." Another, u/StentGuy, said: "Back to work in three days. Needed another stent after 18 months."
Those stories aren’t outliers. They reflect the trade-offs. PCI gives you speed. CABG gives you peace of mind.
There’s no perfect choice. But there is a right one-for your body, your life, and your future.
What happens if you don’t choose?
Some people delay. They hope medication will be enough. But if your arteries are significantly blocked, medications alone won’t prevent a heart attack. PCI and CABG aren’t just about comfort-they’re about survival.
Left untreated, complex coronary disease leads to heart failure, sudden cardiac arrest, or death. Both procedures reduce that risk. The question isn’t whether to intervene-it’s how to intervene.
Is PCI safer than CABG?
PCI has lower immediate risks-less bleeding, no open surgery, lower stroke risk in the first 30 days. But CABG has better long-term outcomes for complex disease. Safety depends on your health, your anatomy, and your goals. For a 70-year-old with diabetes and three blocked arteries, CABG is safer over five years. For a 50-year-old with one simple blockage, PCI is the safer choice.
Can you have both PCI and CABG?
Yes. Some patients get a stent first for an urgent blockage, then later have bypass surgery for other arteries. Others get CABG first, then need a stent later if a graft closes. It’s not uncommon, especially if your disease progresses or you have new blockages. Your heart team will monitor you and adjust treatment as needed.
How long do stents last?
Modern drug-eluting stents last 5 to 10 years in most people. But about 5 to 10% need another procedure within five years. The stent itself doesn’t wear out-it’s the artery around it that can re-narrow. That’s why lifelong heart-healthy habits and medications (like aspirin and statins) are critical after PCI.
Does CABG cure heart disease?
No. CABG improves blood flow, relieves symptoms, and reduces heart attack risk, but it doesn’t stop the disease process. If you keep smoking, eating poorly, or not exercising, new blockages can form-even in your grafts. CABG buys you time. But you still need to manage your heart health every day.
What’s the biggest mistake people make when choosing?
Choosing based on recovery time alone. Many patients pick PCI because they want to get back to work fast. But if you have complex disease, you’re likely to need another procedure in a few years. That means more stress, more cost, and more risk. The goal isn’t to avoid surgery-it’s to avoid repeat interventions and death. Think long-term.
Is CABG worth the long recovery?
If you have diabetes, multi-vessel disease, or a high SYNTAX score, yes. The data shows you’re more likely to live longer and stay free of chest pain. The first two months are hard. But most people say the relief after that is worth it. One patient put it this way: "I didn’t want the surgery. But I didn’t want to die either. I’d do it again in a heartbeat."
Next steps: What to do right now
If you’re facing this decision:
- Ask for your SYNTAX score. Don’t accept vague terms like "bad arteries." Get the number.
- Insist on a heart team meeting. Make sure both a cardiologist and a surgeon review your case together.
- Ask: "Will this choice reduce my chance of another procedure or death in five years?" That’s the real metric.
- Get your diabetes, cholesterol, and blood pressure under control-no matter which procedure you choose.
- Plan your recovery. If you pick CABG, arrange help for the first six weeks. If you pick PCI, still take it slow-your heart needs time to heal.
There’s no rush. Take the time to understand your options. Your heart will thank you.


Dave Alponvyr
Stents are great until they're not. Then you're back in the hospital with a new bill and a new scare. I got mine in '21. Needed another in '23. Worth it for the speed, but don't pretend it's permanent.
Cassandra Collins
They don't tell you the stent companies pay doctors to push them. I saw the slides. Big pharma loves quick fixes. CABG is the real deal but they want you to think it's risky. It's not. It's just not profitable enough.
Dan Padgett
Life is like a river. Sometimes you build a dam. Sometimes you dig a new channel. PCI is the dam - quick, cheap, but the water finds a way back. CABG is the channel - harder to make, but it lasts. My uncle had CABG at 62. He’s 78 now, gardening every morning. No stents. Just a scar and a story.
Hadi Santoso
As a guy who grew up in Jakarta but now lives in Texas, I’ve seen both sides. In the US, they push stents like coffee. In my village back home, they wait till the heart gives out. Neither’s ideal. But if you’ve got diabetes and three blocked arteries? Don’t gamble. Go CABG. Your future self will thank you.
Kayleigh Campbell
So let me get this straight - you get a stent, feel amazing for 18 months, then boom, back in the cath lab while your insurance company high-fives? Meanwhile, the guy who took 8 weeks to recover is now hiking Machu Picchu. I call that a win. Also, why is everyone so scared of a little chest pain? We survived puberty. We can survive sternotomy.
Dylan Smith
I had PCI last year and honestly it was fine but I didn't realize how much I was relying on meds until I forgot my statin for a week and felt like a ghost walking around. The procedure is easy the discipline is hard
sue spark
I’m not a doctor but I read the SYNTAX trial summary and the numbers don’t lie. If your score is over 32 and you’re under 70, CABG isn’t just better it’s the only smart choice. I wish someone had told me that before I picked the stent
Andrew Sychev
I saw a guy on TikTok say CABG is just a glorified plumbing job. I almost cried. This isn’t fixing a leaky faucet. This is rewiring your entire life. And now they want to make it a TikTok trend? What the actual hell is wrong with people?
Arun ana
I’m from India and we don’t have heart teams everywhere. My cardiologist said stent. I asked for a second opinion. Got a surgeon. He said CABG. I went with CABG. Took 3 months to feel normal. Now I play cricket with my nephews. No regrets. 🙏
Kim Hines
My mom had CABG. She cried for two weeks. Then she started baking pies. Now she’s the one reminding everyone to take their meds. I used to think surgery was the end. Turns out it was just the beginning of her second act.
Mike Smith
The heart team model is not bureaucratic - it is essential. As a former cardiac nurse, I’ve seen too many patients choose based on fear or misinformation. The right procedure is not the one that sounds easiest. It’s the one that aligns with your anatomy, your biology, and your long-term goals. Please, do not rush this decision.
Joanna Ebizie
You people act like CABG is some ancient ritual. It’s 2024. We have robots and lasers. Why are you still talking about chest incisions like it’s 1985? Stents are the future. Get with it.
Elizabeth Bauman
I work at a hospital. We do 200 CABGs a year. I’ve seen the data. The stent guys push stents. The surgeon guys push surgery. But the patients who get both opinions? They live longer. And guess what? The ones who listen to the heart team? They don’t come back. The ones who don’t? They’re the ones in the ER again. Don’t be that guy.
Tiffany Machelski
I had the stent and I’m fine but I didn’t know I’d need to take 5 pills every day for the rest of my life. My doctor said it was fine but I keep wondering if I should’ve just taken the big surgery. Oh well. Too late now. I guess I’ll just keep living.