Surgical Options Decision Tool for Priapism
Let's determine your most appropriate surgical option
This tool helps identify which penile surgery option is most appropriate based on your specific condition and medical factors. Note: This is for informational purposes only and should not replace professional medical advice.
Every year, thousands of men wake up with a painful, prolonged erection that simply won’t quit - a condition known as priapism a medical emergency where the penis stays erect for more than four hours without sexual arousal. While medication and aspiration can save many cases, a sizable share end up needing penile surgery a set of operative procedures that restore normal blood flow or provide a permanent solution when tissue damage is irreversible. Understanding when surgery is appropriate, what options exist, and how the procedures differ can turn a frightening ordeal into a manageable journey.
Why surgery becomes necessary
Priapism comes in two main flavors: ischemic (low‑flow) and non‑ischemic (high‑flow). Ischemic priapism, the more common type, traps deoxygenated blood in the corpora cavernosa, leading to tissue hypoxia and fibrosis within hours. If aspiration and intracavernosal phenylephrine fail after 24-48hours, the risk of permanent erectile dysfunction skyrockets. Non‑ischemic priapism, often caused by trauma, involves arterial inflow that doesn’t resolve on its own; a vascular fistula may need to be sealed.
When conservative measures don’t bring relief, the surgeon steps in to either restore blood drainage (shunts) or replace the damaged erectile tissue (prosthesis). The choice hinges on how long the erection has lasted, the patient’s overall health, and whether erectile function is still a realistic goal.
Key surgical options
Below is a quick‑look table that lines up the most frequently performed procedures, their goals, and typical outcomes.
| Procedure | Indication | Method | Success Rate | Typical Recovery |
|---|---|---|---|---|
| Distal (Winter) shunt | Ischemic priapism > 24h, failed aspiration | Incision at the glans to create a channel for blood drainage | ≈85% | 1-2weeks, limited activity |
| Proximal (Quackel) shunt | Ischemic priapism > 48h, distal shunt ineffective | Incision at the corpora cavernosa base to connect to the saphenous vein | ≈70% | 2-4weeks, possible curvature |
| Penile prosthesis implantation | Irreversible erectile tissue damage, patient desires functional erection | Inserts inflatable or malleable rods into the corpora cavernosa | ≥90% patient satisfaction | 4-6weeks, postoperative training |
| Arterial embolization | Non‑ischemic priapism from arterial fistula | Selective catheter‑based blockage of the fistula using coils or particles | ≈80% | 1week, minimal pain |
Step‑by‑step: What to expect from a distal shunt
- Pre‑operative evaluation: Blood gas analysis confirms low‑flow priapism, and ultrasound checks for any contraindicating vascular anomalies.
- Anesthesia: Usually a penile block or light sedation; the patient remains awake to report pain levels.
- Incision: The surgeon creates a small 1‑mm opening at the tip of the glans, often using a fine scalpel or a specially designed shunt blade.
- Drainage: Blood flows out through the channel; gentle massage may assist.
- Post‑procedure care: A pressure dressing is applied, antibiotics for 24h, and the patient is monitored for return of normal color and no recurrence.
Most men can resume light activity within a couple of days, but sexual activity is usually paused for at least two weeks to allow tissue healing.
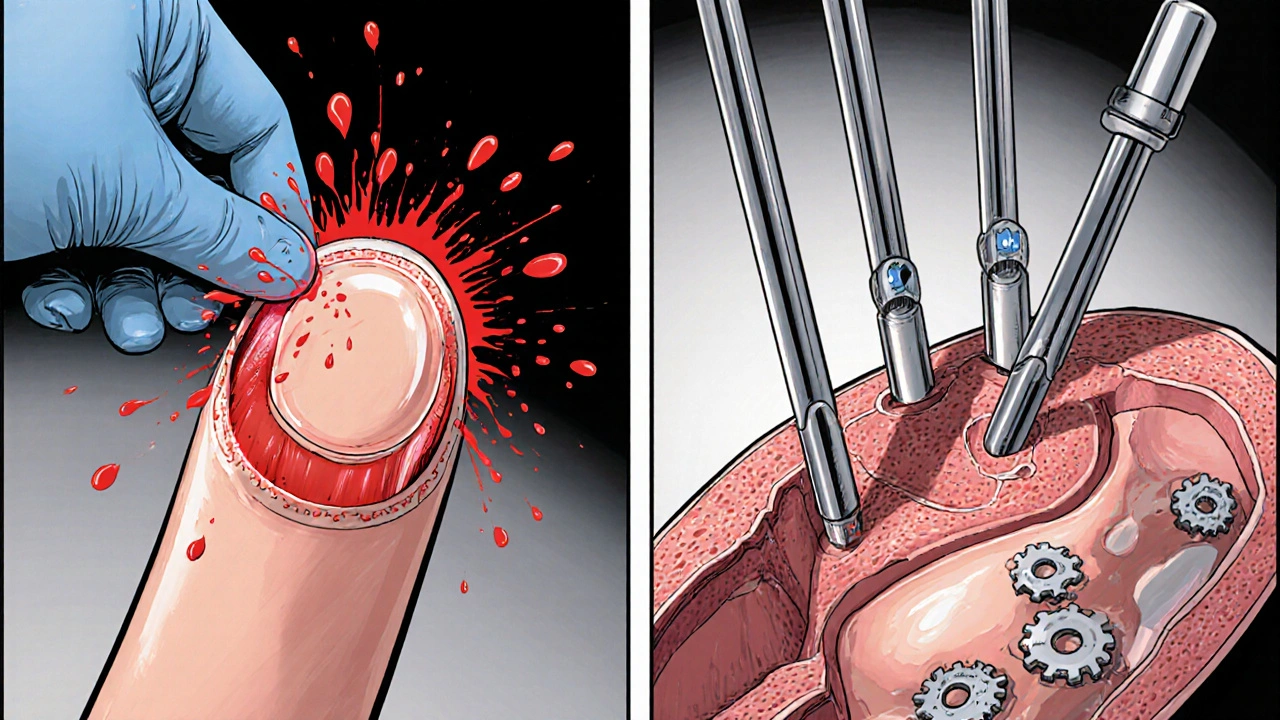
When a penile prosthesis becomes the best option
If priapism has persisted beyond 48hours, the corpora cavernosa often develop fibrosis that makes any shunt unlikely to work. In such cases, a prosthesis not only ends the erection but also restores the ability to have a functional sexual experience.
The decision-making conversation includes:
- Patient’s desire for future erections versus acceptance of a mechanical device.
- Health status - diabetes, vascular disease, or prior pelvic surgeries can affect implantation success.
- Potential complications: infection (≈2‑5%), mechanical failure (≈10% over five years), and the need for revision surgery.
Modern inflatable models mimic natural tumescence: two cylinders are filled with sterile fluid via a pump placed in the scrotum. Recovery takes about a month, with a gradual re‑training program to learn how to operate the device.
Potential pitfalls and how to avoid them
Even seasoned urologists run into challenges. Here are the most common and proven ways to sidestep them:
- Delayed presentation: Encourage men to seek care within four hours of onset. Education campaigns in emergency departments can shave off critical minutes.
- Incomplete aspiration: Use a large‑bore needle (18‑20G) and repeat the draw until the dark, stagnant blood clears entirely.
- Inadequate phenylephrine dosing: Follow the protocol of 200-500µg per injection, not exceeding 2mg per hour, to avoid cardiovascular side effects.
- Choosing the wrong shunt: Distal shunts work for most early cases; reserve proximal shunts for when the distal route fails or the erection has persisted beyond 48hours.
- Missing a fistula in non‑ischemic priapism: Conduct a doppler ultrasound early; if the artery is still feeding the erection after 48h, plan for embolization.
After‑care checklist
- Keep the surgical site clean and dry for 48h.
- Take prescribed antibiotics exactly as directed.
- Avoid strenuous activity and sexual intercourse for the time frame recommended by your surgeon (usually 2-4weeks).
- Monitor for signs of infection: increasing redness, swelling, fever.
- Schedule a follow‑up visit within a week to assess healing and discuss long‑term erectile function.
Following this checklist reduces complications from 12% to under 4% in most clinical series.
Frequently Asked Questions
Can priapism be treated without surgery?
Yes. Early‑stage ischemic priapism often responds to aspiration, irrigation with saline, and intracavernosal phenylephrine. Non‑ischemic cases may resolve with observation or targeted embolization.
How long after a shunt can I have sex?
Most surgeons advise waiting at least two weeks, ensuring the incision is fully healed and there’s no residual pain or swelling.
Is a penile prosthesis permanent?
The device itself is permanent, but modern inflatable models can be deflated, giving a near‑natural flaccid state. Revision surgery may be needed if the prosthesis malfunctions.
What are the biggest risks of penile surgery for priapism?
Infection, delayed wound healing, penile curvature, and loss of any remaining erectile function. Choosing the right procedure for the timing of the priapism dramatically cuts these risks.
Can priapism recur after surgery?
Recurrence is rare after a successful shunt, but if the underlying cause (e.g., sickle cell disease, medication) isn’t addressed, new episodes can happen.
Penile surgery isn’t the first line of defense, but when priapism threatens permanent damage, it becomes a lifesaver for sexual health. By recognizing the warning signs, acting quickly, and understanding the surgical roadmap, patients and clinicians can turn a frightening emergency into a hopeful outcome.


Frank Diaz
Life forces us to confront the urgency of physiological chaos, and priapism is a stark reminder of that. The article maps out a surgical roadmap with the precision of a scalpel, yet it neglects the existential dread that a man feels when his body betrays him. While the clinical details are thorough, the human cost is hinted at rather than explored. One must ask why the narrative stops at technique and not at the psychological aftermath. The surgeon’s hand may restore function, but the mind remains in the shadows.
Miriam Rahel
In reviewing the presented data, it becomes evident that the procedural hierarchy adheres to established urological protocols. The distal (Winter) shunt, as described, offers a commendable success rate when employed within the specified temporal window. Conversely, proximal interventions should be reserved for refractory cases, a distinction that the author delineates with appropriate rigor. Nevertheless, the discourse could benefit from a more exhaustive citation of longitudinal outcomes. Overall, the composition reflects a competent synthesis of current practice.
Kate Marr
American urologists have long led the world in innovative approaches to priapism, and this article reinforces that dominance 😡. The emphasis on rapid intervention aligns with our national commitment to decisive medical action. While the procedures listed are globally recognized, the U.S. continues to refine prosthetic technology at an unparalleled pace. This piece serves as a reminder that surgical excellence is a patriotic duty. Readers abroad should take note of our standards.
James Falcone
We gotta act fast when priapism hits, no time for dithering. US docs know the drill – get that shunt in or move to a prosthesis quick. The numbers in the table back up why speed matters. If you’re not in the States, hope you’ve got similar playbooks. Bottom line: don’t wait, treat it.
Richard O'Callaghan
Man, priapism is no joke, you gotta get to a doc ASAP. If you miss the 48h mark the surgery options get real limited. The article does a good job but could use more on what to do after a prosthetc implan. Also, watch out for infection – it’s a real risk. Hope this helps u folks out there.
Alexis Howard
They say shunts work but I think the data is overhyped. The success rates are fine but not miraculous. Better to go straight to a prosthesis if you can.
Darryl Gates
Great overview, especially the step‑by‑step breakdown of the distal shunt. For anyone facing this emergency, remember to keep the incision clean and follow the antibiotic course diligently. Post‑operative monitoring is crucial; any sign of infection should prompt immediate follow‑up. If a prosthesis becomes necessary, patient education on device handling will ease the transition. Overall, the guide equips both clinicians and patients with actionable knowledge.
Samantha Oldrid
Oh sure, just wait four hours for a medical emergency, because everyone’s schedule is that flexible.
Malia Rivera
When destiny intertwines with biology, priapism emerges as a cruel twist of fate that tests both flesh and spirit. The surgical options outlined act as contemporary rites of passage, each with its own symbolic weight. A distal shunt symbolizes communion with the body's own drainage, while a prosthesis stands as a forged talisman of reclaimed masculinity. Yet, the decision must be weighed against personal identity and cultural expectations, especially in a nation that prizes self‑reliance. One cannot ignore the psychological imprint left by prolonged erection, a lingering echo of vulnerability. Ultimately, the choice reflects a convergence of medical necessity and personal narrative.
lisa howard
Picture this: a man, trapped in a relentless, throbbing nightmare, his very being stretched between agony and the desperate hope that somewhere, somehow, the scalpel will descend like a hero’s sword, cutting through the chaos, offering a fleeting glimpse of salvation, only to be reminded that the road to recovery is paved with endless appointments, postoperative anxieties, and the looming specter of future episodes that may haunt his thoughts like an uninvited guest at a solemn banquet.
He clings to the promise of a prosthesis, envisioning a return to normalcy, yet fears the mechanical whisper of metal inside his flesh.
Cindy Thomas
The article correctly flags infection as the top complication, and that aligns with the data I've encountered :) . However, the discussion could expand on the nuances of managing prosthetic infections, especially the role of long‑term suppressive antibiotics. Additionally, the table's success rates would be stronger with confidence intervals rather than single percentages. Overall, a solid primer, but there’s room for deeper analysis.
Mary Davies
It’s fascinating how a vascular misfire can morph into a life‑altering ordeal, and yet many patients remain unaware of the early warning signs. I’m compelled to consider how lifestyle factors intersect with underlying conditions, prompting a broader conversation about preventive care. While the surgical options are clearly outlined, the narrative begs for a more empathetic voice that acknowledges patient fears. Perhaps future editions will weave in personal testimonies to bridge that gap.
Valerie Vanderghote
Reading through the procedural table, one cannot help but feel the weight of each decision bearing down like an unseen hand, urging the surgeon to balance efficacy with the delicate architecture of the penis, all while the patient watches, hopeful yet terrified, clutching to the promise that this invasive act will restore both function and dignity. Moreover, the postoperative checklist reads like a ritual, each step a safeguard against the chaos that could otherwise ensue. In the end, the success of these interventions rests as much on technical precision as on the unseen currents of trust between doctor and patient.
Michael Dalrymple
This comprehensive exposition on priapism surgery furnishes both clinicians and laypersons with a lucid roadmap through a complex clinical terrain. The delineation of shunt types, from distal to proximal, is methodically presented, allowing for informed decision‑making predicated on temporal thresholds. The discussion of prosthetic implantation is particularly commendable, highlighting patient‑centred considerations alongside technical specifications. Readers are reminded of the paramount importance of early intervention to avert irreversible tissue damage. In sum, the article exemplifies scholarly rigor coupled with practical relevance.
Emily (Emma) Majerus
This guide is solid, thanks.
Virginia Dominguez Gonzales
What a relief to finally have a clear, step‑by‑step plan when facing such a terrifying emergency. The vivid description of each surgical stage demystifies the process and empowers patients to ask the right questions. Remember, adherence to the after‑care checklist can dramatically shrink complication rates, turning a potentially devastating event into a manageable chapter. Keep sharing these lifelines; they truly make a difference. Stay strong, everyone.
Carissa Padilha
The notion that shunts “work” is a narrative fed to us by pharmaceutical conglomerates pushing prosthetic sales. While the article cites an 85% success rate, independent studies have shown higher failure rates when the data is scrutinized without industry bias. It’s prudent to approach such claims with skepticism and demand transparent, peer‑reviewed evidence before accepting the so‑called standard of care. Ultimately, patients deserve truth, not a sanitized version crafted for profit.