When a doctor prescribes a generic drug, they expect it to work just like the brand-name version. That’s the whole point - same active ingredient, lower cost. But more and more clinicians are starting to ask: Are we really getting the same quality? The answer isn’t as simple as regulators claim.
What’s really in that pill?
Generic drugs aren’t made in one clean lab under one roof. They’re stitched together across continents. The active ingredient might come from a factory in Hyderabad, the filler from a plant in New Jersey, the coating from a facility in Shanghai, and the final packaging done in Mexico. Only one company name appears on the label - but that company may have never touched the actual medicine. This fragmentation makes it nearly impossible to track where things go wrong.And it’s not just complexity - it’s cost pressure. As older generics lose patent protection, manufacturers compete by slashing prices. To stay profitable, many outsource production to countries where labor and regulatory oversight are cheaper. The result? A race to the bottom. One study found that generic drugs made in India were linked to 54% more severe adverse events - including hospitalizations and deaths - than identical drugs made in the U.S. That’s not a small difference. That’s a red flag.
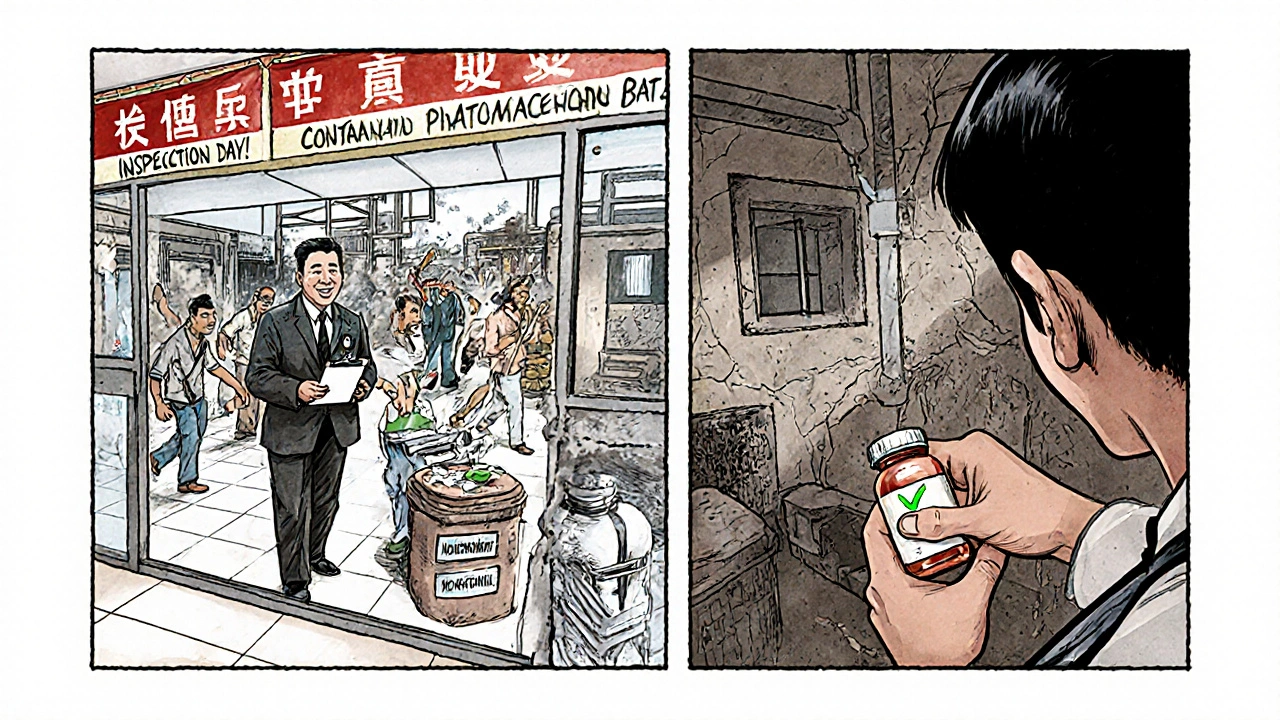
Inspections that don’t inspect
The FDA says the U.S. drug supply is among the safest in the world. And technically, they’re right - for U.S.-based facilities. American plants get unannounced inspections. If something’s off, inspectors show up without warning. Overseas? Not so much. Factories in India and China often get scheduled visits, sometimes weeks in advance. That gives manufacturers time to clean up, hide problems, or temporarily ramp up quality control just for the inspection.Professor Robert S. Gray from Ohio State University put it plainly: “It’s like having a fire marshal come by only when you know they’re coming.” That’s not oversight. That’s theater.
And it’s not just about inspections. The FDA requires generics to prove bioequivalence - meaning they deliver the same amount of active ingredient at the same rate as the brand. But bioequivalence doesn’t guarantee consistency over time. A pill might work fine on day one, but degrade faster in humid conditions. Or the inactive ingredients - the fillers, binders, coatings - might react differently in different climates. These aren’t just “fillers.” They’re critical to how the drug dissolves, absorbs, and works in your body.
Older drugs, bigger risks
The problem gets worse with older generics. Drugs like metformin, levothyroxine, or hydrochlorothiazide have been on the market for decades. They’re cheap. Everyone uses them. But because they’re no longer profitable for big pharma, only low-cost manufacturers bother making them. And those manufacturers often use outdated equipment, minimal quality controls, and supply chains stretched thin.Researchers at Duke-Margolis Center found that these older generics are the leading cause of drug shortages. Why? Because when a factory in India has a quality failure - say, contaminated batches or inconsistent dissolution rates - there’s no backup. The entire U.S. supply can crash overnight. Patients with heart conditions, epilepsy, or thyroid disorders don’t get their meds. Some go without. Others switch to alternatives that don’t work as well. The consequences? Higher mortality, delayed cancer treatments, medication errors.
Is the FDA keeping up?
The FDA has over 1,300 staff dedicated to drug quality. That sounds impressive. But they’re responsible for inspecting thousands of facilities across more than 150 countries. They can’t be everywhere. And while they’ve started pushing for advanced manufacturing technologies - like real-time monitoring and continuous production - adoption is slow. Why? Because these systems cost millions upfront. And for a company making pennies per pill, that’s a hard sell.Here’s the kicker: over 80% of drugs made with advanced manufacturing are produced in the U.S. That’s not a coincidence. It’s proof that better technology leads to better quality. But until there’s financial incentive to upgrade, most overseas factories will stick with old, unreliable methods. And patients will keep paying the price.
What clinicians are seeing
Doctors aren’t just reading studies. They’re seeing it in real time. A pharmacist in Ohio reported multiple patients switching from one generic levothyroxine to another - same dose, same label - and suddenly developing palpitations, weight loss, or anxiety. The only difference? The manufacturer. Another clinician in Texas noticed a spike in seizures among epilepsy patients after a new generic version hit the shelves. The FDA didn’t issue a recall. The drug was “bioequivalent.” But the patients weren’t stable.Dr. Iyer, a specialist in global health, says the solution isn’t more regulation - it’s smarter purchasing. “Procurers need to stop buying the cheapest drug,” he says. “They need to buy the best drug. If a manufacturer can prove quality assurance, they should get the contract. If they can’t, they shouldn’t be in the market.”
And it’s not just generics. Dr. Guzman reminds us: “Branded drugs can be substandard too.” But the difference? Brand-name manufacturers have more to lose. They’re watched. They’re scrutinized. Generics? Not so much.
Domestic production: a realistic fix?
The University of Wisconsin School of Pharmacy makes a simple point: If we made more generic drugs in the U.S., we’d have fewer quality concerns, fewer shortages, and a more resilient supply chain. It sounds ideal. And it’s not fantasy. The technology exists. The workforce exists. The infrastructure exists.The problem? Profit margins. A pill made in Ohio costs three times as much as one made in India. Hospitals and Medicaid programs don’t want to pay more. But what’s the real cost? A patient hospitalized because their blood pressure drug didn’t work? A cancer patient missing a dose because the generic ran out? Those costs aren’t on the pharmacy ledger - they’re on the hospital’s balance sheet, and in the patient’s life.
What’s next?
There’s no easy fix. But there are clear steps forward:- Make manufacturing location public. Patients and doctors deserve to know where their drugs come from.
- Require unannounced inspections for all facilities - no exceptions.
- Incentivize advanced manufacturing in the U.S. through tax breaks, grants, or guaranteed purchase agreements.
- Stop equating “bioequivalent” with “safe and consistent.” Quality isn’t a single test. It’s a system.
The FDA says the system works. Clinicians say they’re seeing the cracks. And patients? They’re just taking their pills - hoping they’ll work.
Are generic drugs really as good as brand-name drugs?
In theory, yes - they’re required to have the same active ingredient and meet bioequivalence standards. But in practice, quality varies widely depending on who made it, where it was made, and how old the drug is. Some generics work perfectly. Others cause unexpected side effects or fail to control symptoms. The difference often comes down to manufacturing practices, not the drug itself.
Why do some generic drugs cause more side effects than others?
It’s usually not the active ingredient. It’s the inactive ingredients - the fillers, coatings, or binders - or how consistently the drug dissolves in the body. A pill made in a factory with outdated equipment might break down too slowly or too quickly. A batch made under poor conditions might have impurities. These aren’t always caught in standard testing, which is why patients report different reactions to the same generic drug from different manufacturers.
Can I tell where my generic drug was made?
Not easily. The label only shows the distributor’s name, not the manufacturer’s location. Some pharmacies can tell you if you ask, but most don’t track that information. The FDA doesn’t require manufacturers to disclose origin on the label. That’s changing - but slowly. Advocates are pushing for mandatory country-of-origin labeling on all prescription drugs.
Should I avoid generic drugs altogether?
No. For most people, generics are safe and effective. But if you’re on a medication where small changes in dosage or absorption matter - like thyroid drugs, seizure meds, or blood thinners - pay attention. If you notice new side effects after switching generics, talk to your doctor. You may need to stick with one brand or manufacturer. Don’t assume all generics are equal.
Is the U.S. going to bring generic manufacturing back home?
There’s growing pressure to do so - especially after drug shortages during the pandemic and rising concerns over foreign supply chains. Some government programs are offering funding to restart domestic production, and advanced manufacturing tech is making it more cost-effective. But without policy changes that reward quality over price, most companies will keep outsourcing. It’s not impossible - it just needs political will and patient advocacy.


Kathryn Ware
I’ve had patients switch generics and suddenly develop weird palpitations or anxiety-same dose, same label, totally different experience. It’s terrifying. I’ve started asking pharmacies for the manufacturer name, and honestly? Most don’t even track it. We’re flying blind. And don’t get me started on levothyroxine. One batch makes you feel like a superhero, the next? You’re shaking, sweating, and wondering if you’re having a panic attack or just bad meds. 🤯
kora ortiz
This is why we need mandatory country of origin labeling on every prescription bottle. No more hiding behind corporate names. Patients deserve to know if their life-saving drug was made in a factory with scheduled inspections and outdated equipment. Stop pretending bioequivalence means safety. It doesn’t. And if we want real change, we stop rewarding the cheapest bid and start paying for quality. Period.
Jeremy Hernandez
Big Pharma and the FDA are in bed together. They don’t care if your thyroid meds don’t work because they’re not the ones taking them. The whole system is rigged. India and China are dumping substandard crap because they know the FDA won’t show up unannounced. And guess who pays? Us. The poor. The elderly. The ones who can’t afford brand names. This isn’t a supply chain issue-it’s a conspiracy. They want us dependent on foreign pills so they can control the market. Wake up.
Tarryne Rolle
Isn’t it ironic that we demand purity in our food, our water, our air-but when it comes to the chemicals we ingest to stay alive, we accept whatever’s cheapest? We’ve outsourced not just manufacturing but moral responsibility. The pill doesn’t care if it was made in Ohio or Hyderabad. But we do. And maybe that’s the real problem-we’ve stopped caring about the human behind the dosage. We treat medicine like a commodity, not a covenant.
Kyle Swatt
Look, I get it-cheap meds save lives. But we’re playing Russian roulette with people’s hearts, brains, and kidneys. It’s not about nationalism. It’s about integrity. A pill isn’t just a chemical-it’s a promise. That promise gets broken when the coating cracks in humid shipping containers or the filler clumps because the mixer’s from 1997. We’ve built a system that rewards speed over soul. And now we’re surprised when people get sick? Nah. We built this. We chose profit over precision. And that’s on all of us.
Deb McLachlin
The data presented here is compelling and aligns with multiple peer-reviewed studies on generic drug variability. The key issue lies not in the active pharmaceutical ingredient but in the physicochemical properties of excipients and manufacturing consistency. Bioequivalence testing is a snapshot, not a longitudinal guarantee. The lack of real-time dissolution monitoring in overseas facilities is a critical regulatory gap. I strongly support the proposed policy interventions, particularly unannounced inspections and incentivized domestic advanced manufacturing.
saurabh lamba
USA always thinks they’re better. India makes 40% of the world’s generics. You think your $10 pill is safe? Your FDA is broke. Your inspectors are overworked. We make good medicine. You just don’t like paying less. 😎
Kiran Mandavkar
You think this is bad? Wait until you see what’s coming from Bangladesh and Vietnam. The FDA’s inspection regime is a joke. But you Americans have the nerve to lecture us? You don’t even have universal healthcare. You let people die because they can’t afford insulin. Now you’re mad because your cheap generics might not dissolve properly? Grow up. This isn’t about quality. It’s about your entitlement.
Eric Healy
Bro the FDA is totally asleep at the wheel. I work in a pharmacy and we get shipments where the pills look different. Same name same dose but one batch is white and the other is kinda yellow? And the pills crumble if you look at them wrong. And no one says anything. They just say 'it's bioequivalent' like that means anything. Smh.
Shannon Hale
MY COUSIN HAD A SEIZURE BECAUSE HER GENERIC EPILEPSY MED WAS MADE IN A FACTORY THAT USED A BROKEN MIXER. THE FDA DIDN’T RECALL IT BECAUSE IT WAS ‘WITHIN RANGE.’ RANGE? RANGE?! MY COUSIN WAS IN A HOSPITAL FOR THREE WEEKS. THIS ISN’T A LOGISTICS PROBLEM. THIS IS A CRIME. WE NEED TO BURN THE WHOLE SYSTEM DOWN AND START OVER.
Holli Yancey
I’ve been on levothyroxine for 12 years. I’ve switched generics twice. The first time I felt like I was drowning in my own skin. The second time I couldn’t sleep for a week. I switched back to the original brand and everything stabilized. I’m not anti-generic. I’m pro-stability. If a drug works for you, don’t mess with it. And if you’re told it’s ‘the same’-ask for the manufacturer. It matters more than you think.
Gordon Mcdonough
AMERICA IS BEING SABOTAGED. FOREIGN FACTORIES ARE DELIBERATELY MAKING BAD DRUGS TO MAKE US WEAK. THE CHINESE AND INDIANS KNOW WE’RE DEPENDENT ON THEM. THEY’RE NOT JUST MAKING PILLs-THEY’RE MAKING SLAVES. WE NEED TO BAN ALL FOREIGN DRUGS. BUILD OUR OWN. PROTECT OUR PEOPLE. THIS ISN’T A HEALTH ISSUE-IT’S A WAR.
Jessica Healey
My grandma’s blood pressure meds went from perfect to terrifying in one week. She started fainting. We found out the manufacturer changed. She went back to the old one and boom-back to normal. No one at the pharmacy even blinked. They just shrugged and said 'it's the same.' Same? Same? My grandma almost died because some factory in India decided to cut corners. This isn’t healthcare. It’s a gamble.
Levi Hobbs
My dad’s on metformin. He’s been on the same generic for years. Last month, he got a new bottle. Started feeling dizzy, nauseous, his legs felt like lead. We called the pharmacy. They said it was the same drug. I looked up the manufacturer code. Different company. Same name. Different country. We switched back. He’s fine now. This isn’t just about cost. It’s about trust. And we’ve lost it.
henry mariono
I don’t have a solution. But I do know this: if a drug affects your heart, your brain, or your ability to breathe, it shouldn’t be treated like a bulk commodity. We treat our pets better than this. Maybe we need to start there.