For years, doctors avoided prescribing statins to patients with liver disease. The fear wasn’t about heart attacks-it was about the liver. Many believed statins could damage an already fragile organ. But today, that thinking is outdated. New evidence shows statins aren’t just safe for people with liver disease-they may actually help protect the liver while cutting heart attack risk.
Why Statins Were Once Avoided
Statins, like atorvastatin and rosuvastatin, were developed to lower LDL cholesterol-the "bad" kind that clogs arteries. By the 1990s, they became the go-to treatment for heart disease. But liver disease patients were left out. Why? Because statins are processed by the liver. Doctors worried they’d overload it. That concern came from old data. Early case reports mentioned rare liver enzyme spikes. But those weren’t caused by statins. They were coincidental. In reality, severe liver injury from statins happens in about 1 in 100,000 patients per year. That’s rarer than being struck by lightning.How Statins Actually Work
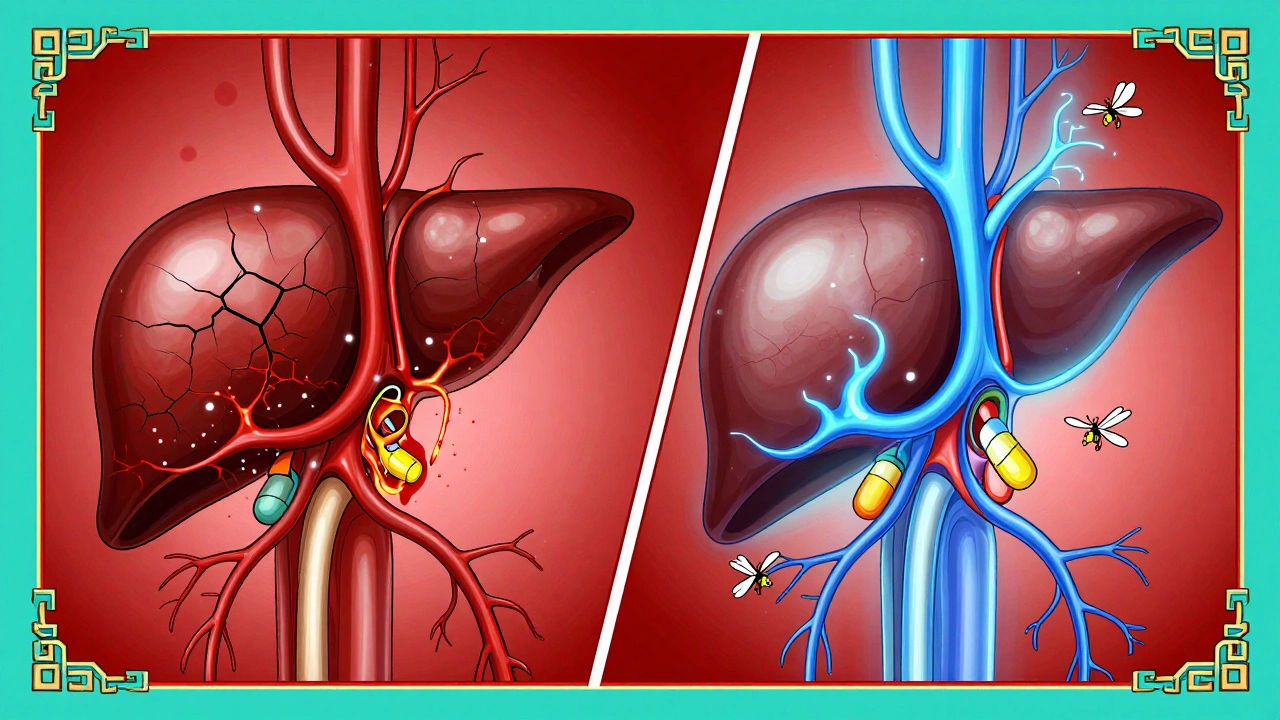
Statins block HMG-CoA reductase, the enzyme your liver uses to make cholesterol. When that enzyme slows down, your liver pulls more LDL out of your blood to make up for the loss. That’s how LDL drops by 25% to 60%, depending on the dose and type of statin. But that’s not all. Statins also reduce inflammation. They calm down immune cells in blood vessels, improve blood flow, and help stabilize plaque so it doesn’t rupture. For someone with liver disease, this matters. Chronic inflammation from fatty liver or cirrhosis speeds up scarring. Statins fight that. Studies in rats with cirrhosis showed simvastatin improved blood flow through the liver by 20% and lowered resistance in liver vessels by 14% within 30 minutes. Human studies confirmed this. In one trial with 30 cirrhotic patients, those on simvastatin had better liver blood flow and lower pressure in the portal vein-the main blood vessel to the liver. That’s huge. High portal pressure causes dangerous bleeding in the stomach and esophagus.Statins Don’t Hurt the Liver-They May Help It
The biggest myth? That statins cause liver damage. They don’t. Multiple large studies prove it. The JUPITER trial followed 18,000 people for two years. Half took rosuvastatin. Half took a placebo. Rates of liver problems? Identical. The EXCEL trial with 8,000 patients on lovastatin found zero cases of hepatitis. Even in patients with fatty liver disease, statins didn’t worsen liver enzymes. In fact, many saw them improve. A 2023 study in Gastroenterology Research tracked over 1,200 patients with compensated cirrhosis. Those taking statins had:- 22% lower risk of liver decompensation
- 38% lower risk of variceal bleeding
- 26% lower risk of death
Who Should Take Statins? Even With Liver Disease
You don’t need a healthy liver to benefit from statins. Guidelines from the American Heart Association and the European Association for the Study of the Liver now say:- Statins are safe for non-alcoholic fatty liver disease (NAFLD)
- Statins are safe for compensated cirrhosis (Child-Pugh A and B)
- Statins can be used in patients with mild to moderate enzyme elevations-up to three times the normal limit
Which Statin Is Best for Liver Disease?
Not all statins are the same. Some rely heavily on liver enzymes (CYP3A4) to break down. That’s a problem if you’re on other meds or your liver is weak. Here’s what works best:- Rosuvastatin-mostly cleared by the kidneys, not the liver. Safe even with advanced disease.
- Pravastatin-also low liver metabolism. Good for older patients on multiple drugs.
- Atorvastatin-effective but processed by the liver. Use lower doses if you have cirrhosis.
- Avoid simvastatin and lovastatin in advanced disease-they’re heavily metabolized by CYP3A4.
What About Side Effects?
The most common issue with statins? Muscle aches. About 1 in 10 people report this. But it’s rarely serious. In liver disease patients, muscle symptoms are no more common than in healthy people. One Reddit thread with 58 cirrhosis patients found 84% had no liver-related side effects. Only 16% saw a small, temporary rise in liver enzymes-and those went back to normal without stopping the statin. The real problem? Doctors still hesitate. A 2023 survey found that 31% of liver disease patients had to push for a statin prescription. Some were told, "It’s too risky." That’s outdated advice.What If You’re Already on Other Medications?
Many liver disease patients take multiple drugs-diuretics for fluid, beta-blockers for portal pressure, antivirals for hepatitis. Drug interactions are a real concern. Rosuvastatin and pravastatin are the safest choices here. They don’t rely on the CYP450 system, so they don’t interfere with most other meds. Avoid grapefruit juice. It blocks the enzymes that break down some statins and can raise their levels dangerously. If you’re on antivirals for hepatitis C or B, talk to your doctor. Some newer antivirals can be safely combined with statins. Others need spacing or dose adjustments. But stopping statins isn’t the answer.
The Bigger Picture: Saving Lives Beyond the Heart
Statins aren’t just heart pills. For people with liver disease, they’re multi-tool drugs. A 2023 study in JAMA Network Open followed nearly 50,000 patients with chronic liver disease. Those on high-intensity statins had a 17% lower risk of dying from any cause. Liver-related deaths dropped by 28%. Why? Because statins reduce inflammation, improve blood flow, prevent bleeding, and slow fibrosis. They’re one of the few treatments that address both heart and liver problems at once. The cost savings are real, too. The Institute for Clinical and Economic Review estimated statins save $1,200 to $3,500 per patient per year by preventing hospitalizations for bleeding, ascites, and liver failure.What’s Next?
The STATIN-CIRRHOSIS trial (NCT04567891) is now recruiting patients with decompensated cirrhosis. Results are expected in late 2025. If the data holds, it could change guidelines again-this time to recommend statins even for the sickest patients. Right now, the evidence is clear. Statins are not dangerous for liver disease. They’re one of the most underused tools we have to extend life and improve quality. If you have liver disease and a history of heart attack, stroke, high cholesterol, or diabetes-you should be on a statin. Not because it’s trendy. But because the science says it saves lives.What If Your Doctor Says No?
If your doctor refuses to prescribe a statin because of your liver disease, ask for this:- The 2022 AASLD Clinical Guidance on Liver Disease
- The American Heart Association’s 2018 Scientific Statement on statins in liver disease
- The European Association for the Study of the Liver (EASL) 2021 guidelines
Are statins safe if I have cirrhosis?
Yes, statins are safe for compensated cirrhosis (Child-Pugh A and B). Multiple large studies show no increased risk of liver damage. In fact, statins reduce portal pressure, lower risk of bleeding, and improve survival. For advanced cirrhosis (Child-Pugh C), start with low doses of rosuvastatin or pravastatin and monitor closely-but they’re still recommended if you have cardiovascular risk.
Do statins raise liver enzymes?
Rarely. In clinical trials, statins cause no more liver enzyme elevations than placebo. Mild, temporary increases happen in less than 5% of patients, and they almost always resolve without stopping the medication. If enzymes rise above three times the upper limit of normal, check for other causes-like worsening liver disease or another drug-before assuming it’s the statin.
Can I take statins if I have fatty liver disease?
Absolutely. Fatty liver disease (NAFLD) is one of the best reasons to take a statin. These patients have a much higher risk of heart disease. Statins lower LDL, reduce inflammation, and may even reduce liver fat and fibrosis. Guidelines from the American Heart Association and EASL strongly support statin use in NAFLD patients with cardiovascular risk factors.
Which statin is safest for liver disease?
Rosuvastatin and pravastatin are the safest choices. They’re cleared mainly by the kidneys, not the liver, so they’re less likely to build up in people with liver impairment. Avoid simvastatin and lovastatin in advanced disease because they rely on liver enzymes that may be slowed. Atorvastatin is fine at lower doses.
Do I need regular liver tests while on statins?
No. The American Heart Association no longer recommends routine liver enzyme monitoring for statin users. Baseline tests before starting are fine, but monthly or quarterly checks aren’t needed. If you feel well and have no symptoms, no blood work is required. Focus on cholesterol levels and cardiovascular risk instead.
Can statins help prevent liver cancer?
Emerging data suggests statins may reduce liver cancer risk in patients with cirrhosis. A 2023 meta-analysis showed a 30% lower incidence of hepatocellular carcinoma in statin users. The mechanism likely involves reduced inflammation and fibrosis. While not yet a formal indication, this is one of the most promising areas of future research.

Graham Abbas
It's wild how we used to treat statins like poison for the liver, when really they're more like gardeners pruning the bad branches.
It's not about avoiding stress on the organ-it's about giving it the right kind of support. The liver isn't fragile-it's misunderstood.
And honestly? If we applied this same logic to every drug we thought was 'hard on the liver,' we'd be stuck with nothing but aspirin and hope.
Statins don't break the liver. They help it breathe again.
George Taylor
Okay, but... have you actually read the FDA’s Adverse Event Reporting System? Because ‘rare’ doesn’t mean ‘never.’
And ‘statins improve liver function’? That’s not a conclusion-it’s a wishful headline.
Also, why is every study funded by Big Pharma? Coincidence? I think not.
And don’t get me started on ‘no need for liver tests’-that’s just asking for disaster.
And why is everyone suddenly an expert? I’ve seen patients crash after being told ‘it’s fine.’
It’s not about fear-it’s about caution. And caution is being thrown out the window like yesterday’s newspaper.
Evelyn Pastrana
So let me get this straight-you’re telling me the same pill that keeps my uncle from having a heart attack might also save his liver? And we used to tell people NO? 😅
Y’all are giving me whiplash.
First we say ‘don’t touch statins,’ then we say ‘here, take two and call your liver in the morning.’
Can we just agree that medicine is weird sometimes?
Also, if statins are magic beans, can I get some for my mom with fatty liver? She’s been eating kale and crying since 2018.
Carina M
It is imperative to note that the assertion that statins are universally safe in the context of hepatic impairment is not only premature but potentially perilous.
While certain cohort studies suggest favorable outcomes, they are observational in nature and therefore susceptible to confounding variables.
Moreover, the absence of randomized controlled trials in decompensated cirrhosis renders any clinical recommendation premature.
One must exercise the utmost caution before abandoning established clinical prudence in favor of trend-driven enthusiasm.
Furthermore, the suggestion that routine liver enzyme monitoring is unnecessary contravenes decades of evidence-based hepatological practice.
One cannot simply discard safeguards because the narrative has become palatable.
Tejas Bubane
Statins help liver? Bro you serious? I seen my cousin take it for 3 years and his enzymes went through the roof then he got jaundice
Doctors just wanna push pills
They dont care if you live or die as long as you keep coming back
And now they say no blood tests? Are you kidding me? I bet they dont even check their own liver
Its all money money money
Ajit Kumar Singh
In India we have millions with fatty liver and no access to statins because they are too expensive and doctors are scared to prescribe
But here in the US you have people arguing about whether statins are safe
Meanwhile in rural Bihar people die from bleeding varices because they cant afford a $5 pill
Stop arguing and fix the system first
Statins are not the problem-the inequality is
Larry Lieberman
Wait so statins are like… liver BFFs now? 🤯
Also I just found out they might reduce liver cancer risk? 😳
Okay but can we talk about how wild it is that we thought the liver couldn’t handle them?
Like… our liver is a superhero. It regenerates. It detoxes whiskey. It handles 500+ chemical reactions a second.
Statins are just… chillin’ in the background doing cardio for the whole system.
Also, rosuvastatin = kidney-powered superhero. 🦸♂️💧
Sabrina Thurn
The paradigm shift here is profound: statins are no longer viewed as hepatotoxic agents but as pleiotropic modulators of hepatic hemodynamics and fibrogenesis.
Multiple meta-analyses confirm a reduction in portal hypertension via endothelial nitric oxide synthase upregulation and reduced sinusoidal resistance.
The clinical implication is that statins are not merely cardioprotective-they are antifibrotic, anti-inflammatory, and anti-angiogenic in the context of chronic liver disease.
It’s not anecdotal; it’s pathophysiologically coherent.
And yet, the persistence of outdated guidelines reflects systemic inertia in medical education, not scientific uncertainty.
Patients deserve evidence, not fear.
Anna Roh
So… statins are good now?
Wait, but what about that one guy on Reddit who said his liver exploded?
Also, I read somewhere that statins make you gain weight.
And isn’t cirrhosis supposed to be irreversible?
Why does this feel like a 2018 meme that got a research paper?
Can we just… not?
Tiffany Sowby
Oh great. Another American medical miracle that only works if you have insurance.
Meanwhile, my cousin in Texas got denied statins because her liver enzymes were ‘slightly elevated’-even though she’s got diabetes, high BP, and a 70% chance of a heart attack by 50.
And now you want me to believe this is safe?
It’s not science-it’s privilege.
Statins for the rich, cirrhosis for the poor.
That’s the real story here.
Asset Finance Komrade
It is curious how Western medicine continually re-invents the wheel under the banner of innovation.
Statins were never the answer-they are merely a chemical bandage on a systemic failure.
The real issue is diet, sedentary lifestyles, and industrial food systems.
Prescribing statins to compensate for societal neglect is not progress-it is capitulation.
And to claim they ‘help the liver’ is to confuse symptom management with healing.
The liver does not need a pill. It needs rest.
And we, as a culture, refuse to give it that.
Jennifer Blandford
Okay I’m crying. Not because I’m emotional-because this is the first time I’ve heard someone say something good about my liver.
I’ve been told for 8 years that I have NAFLD and ‘just lose weight’.
But no one said, ‘Hey, here’s a pill that might actually help you live longer.’
My doctor didn’t even mention statins until I brought it up.
So thank you. For the science. For the hope.
And for not treating me like I’m broken.
My liver is still here. And now it has a chance.
Brianna Black
As a hepatology nurse practitioner with 14 years in clinical practice, I can confirm: the evidence is overwhelming.
Statins are not merely tolerated in compensated cirrhosis-they are underutilized.
Our patients on statins have fewer variceal bleeds, fewer admissions for ascites, and longer transplant-free survival.
And yes, we monitor liver enzymes-but not because we fear statins.
We monitor because we care.
And when enzymes rise? We look for other causes-viral flare, alcohol, drug interactions.
Not the statin.
It’s time to stop letting fear dictate care.
Patients deserve better.
Stacy Tolbert
I’ve been on statins for 5 years with cirrhosis.
My liver enzymes? Lower now than when I started.
My portal pressure? Down.
My anxiety? Gone.
Because I finally felt like someone was fighting for me.
Not just my heart.
My liver too.
So if your doctor says no?
Bring this article.
And then bring your own stubbornness.
You’ve got this.