Stem Cell Therapy Comparison Tool
Treatment Options Overview
Immune Reset Approach
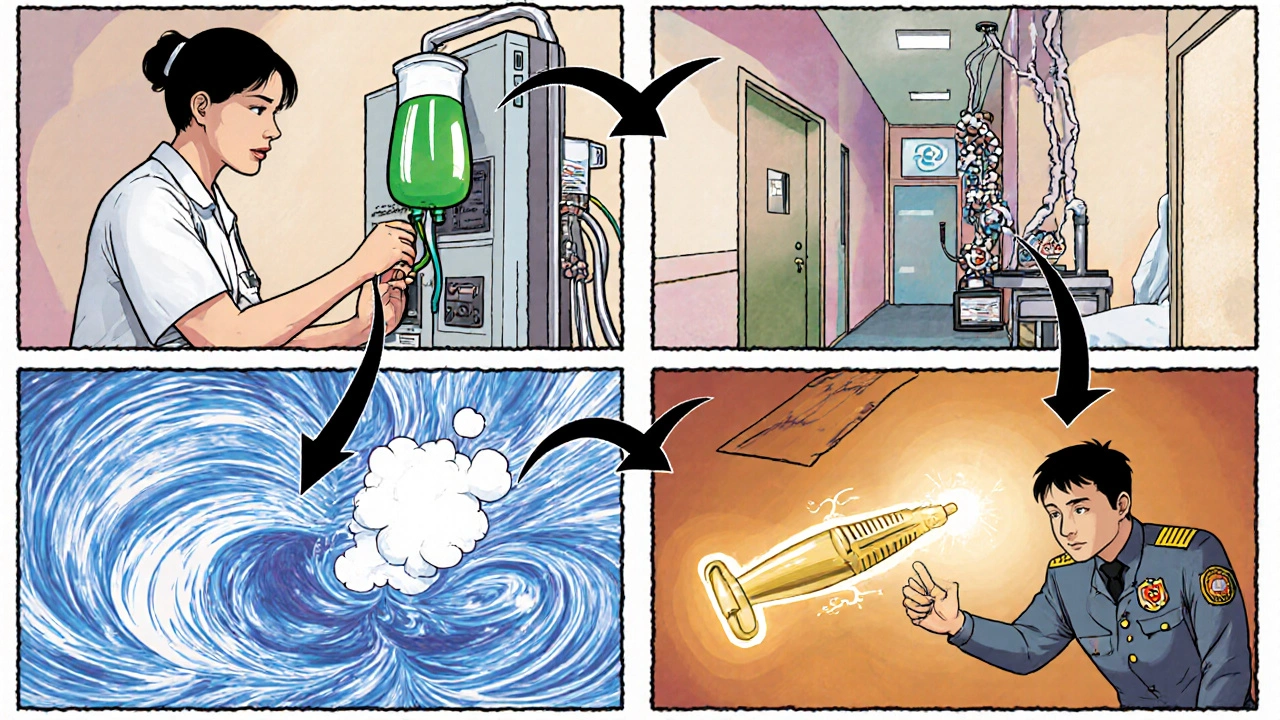
HSCT involves high-dose chemotherapy to wipe out the faulty immune system followed by reinfusion of the patient's own stem cells to rebuild a tolerant immune system.
| Feature | HSCT |
|---|---|
| Primary Goal | Immune reset |
| Annualized Relapse Rate Reduction | ≈ 80% |
| EDSS Improvement (median) | -0.5 to -1.0 |
| Serious Adverse Event Rate | 5-7% (infection, organ toxicity) |
| Procedure Complexity | High (3-4 week hospital stay) |
Eligibility Assessment
Active secondary progressive MS patients must meet the following criteria to be considered for these therapies:
Key Takeaways
- Stem cell therapy, especially autologous hematopoietic stem cell transplantation (HSCT), can halt or even reverse disease activity in active secondary progressive multiple sclerosis (SPMS).
- Mesenchymal stem cell (MSC) infusions are safer but show modest benefit; they are often used when HSCT is not an option.
- Both approaches outperform conventional disease-modifying therapies (DMTs) in short‑term relapse reduction, but long‑term data are still emerging.
- Patient selection hinges on recent relapse activity, MRI‑shown lesion growth, and limited disability (EDSS ≤6.5).
- Regulatory approval varies across Europe; the European Medicines Agency (EMA) classifies HSCT as an advanced therapy medicinal product (ATMP), while NICE provides guidance on funding in the UK.
When talking about cutting‑edge options for stem cell therapy is a regenerative treatment that uses undifferentiated cells to repair or replace damaged tissue, patients with active secondary progressive multiple sclerosis (SPMS) are often the focus.
The promise of stem cell therapy lies in its ability to reset the immune system and foster neuroprotection, two mechanisms that conventional disease‑modifying therapies (DMTs) struggle to achieve simultaneously.
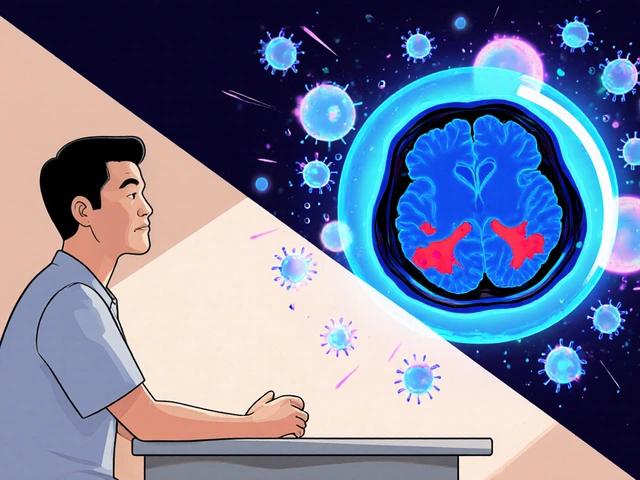
Understanding Active Secondary Progressive MS
Secondary Progressive Multiple Sclerosis is a stage of MS marked by steady neurological decline after an initial relapsing‑remitting phase. "Active" SPMS means the disease still shows inflammatory activity - new relapses or MRI‑visible lesion expansion within the past year. This activity signals that the immune system is still attacking myelin, making patients eligible for immuno‑resetting strategies like stem cell transplantation.
Key clinical markers of activity include:
- At least one documented clinical relapse in the last 12 months.
- New or enlarging T2 lesions on brain MRI.
- Gadolinium‑enhancing lesions indicating blood‑brain‑barrier breach.
How Stem Cell Therapy Works
Stem cell therapy can be split into two main streams for MS:
- Hematopoietic Stem Cell Transplantation (HSCT) is a procedure that harvests a patient’s own blood‑forming stem cells, administers high‑dose chemotherapy to wipe out the faulty immune system, then re‑infuses the harvested cells to rebuild a tolerant immune repertoire.
- Mesenchymal Stem Cell (MSC) therapy is an infusion of multipotent stromal cells derived from bone marrow, adipose tissue, or umbilical cord, aimed at modulating inflammation and supporting neuronal survival.
While HSCT focuses on immune reset, MSCs act more like biological “painkillers” for the nervous system, dampening cytokine storms and releasing growth factors that may repair damaged axons.
Autologous HSCT for Active SPMS
Autologous Transplant is the specific form of HSCT where the patient’s own stem cells are used, eliminating graft‑versus‑host disease risk. The typical protocol involves three steps:
- Mobilization: a drug like cyclophosphamide or G‑CSF pushes stem cells from bone marrow into the bloodstream.
- Collection: apheresis gathers enough CD34+ cells for reinfusion.
- Conditioning: high‑dose chemotherapy (e.g., BEAM or cyclophosphamide + ATG) suppresses the existing immune network.
- Reinfusion: harvested cells are returned, repopulating a “clean” immune system.
Clinical data from the European Blood and Marrow Transplantation (EBMT) registry show that, at five‑year follow‑up, relapse‑free survival reaches 70‑80 % in selected active SPMS patients, with a median EDSS improvement of 0.5‑1.0 points. Mortality rates have dropped below 1 % in high‑volume centers thanks to refined conditioning regimens.
Mesenchymal Stem Cell Therapy: A Safer Alternative
Mesenchymal Stem Cells are multipotent cells that can differentiate into bone, cartilage, and fat, but in MS they are prized for their immunomodulatory secretome. The procedure is less intense:
- Harvest: bone‑marrow or adipose tissue is collected under local anesthesia.
- Expansion: cells are cultured for 2‑3 weeks to reach therapeutic dose (typically 1‑2 × 10⁶ cells per kilogram).
- Infusion: cells are delivered intravenously, often repeated 2‑4 times over six months.
Phase II trials (e.g., the MSC‑MS trial in Spain) report a 30‑40 % reduction in new MRI lesions and a modest improvement in fatigue scores. Importantly, serious adverse events are rare, with most patients experiencing only mild infusion reactions.
Comparing Stem Cell Strategies with Conventional DMTs
| Feature | HSCT | MSC Therapy | Standard DMTs |
|---|---|---|---|
| Primary Goal | Immune reset | Neuro‑protection & immunomodulation | Relapse reduction |
| Annualized Relapse Rate (ARR) Reduction | ≈ 80 % | ≈ 30‑40 % | ≈ 30 % |
| EDSS Improvement (median) | ‑0.5 to ‑1.0 | ‑0.2 to ‑0.5 | 0 (stable) |
| Serious Adverse Event Rate | 5‑7 % (infection, organ toxicity) | <1 % (infusion reaction) | ≈ 2 % (infection, liver issues) |
| Regulatory Status (EU/UK) | Approved as ATMP by EMA for relapsing MS; off‑label for SPMS | Investigational - clinical‑trial use only | Fully licensed |
The table shows that HSCT offers the strongest disease‑modifying effect, but it comes with higher short‑term risk. MSCs sit in the middle - safer, but outcomes are less dramatic. Conventional DMTs remain the baseline for patients with low disease activity.
Practical Considerations for Patients and Clinicians
Choosing a stem cell approach hinges on three pillars:
- Disease Activity: Recent relapses or MRI activity are required for HSCT eligibility.
- Disability Level: EDSS ≤6.5 ensures the patient can tolerate conditioning and mobilization.
- Center Experience: High‑volume transplant centers report lower mortality; the UK's NHS trusts with HSCT programs include London King’s College Hospital and Manchester Royal Infirmary.
Funding in the UK is guided by NICE which recommends HSCT for relapsing‑remitting MS with high activity; for SPMS, funding decisions are made on a case‑by‑case basis, often requiring a health‑technology assessment.
Cost estimates vary: a full HSCT cycle runs between £30,000‑£45,000 in the UK, while MSC infusions can cost £8,000‑£12,000 per treatment round. Private insurance coverage is rare, so many patients explore clinical‑trial enrollment to offset expenses.

Risks, Side Effects, and Post‑Procedure Monitoring
HSCT’s most serious risk stems from the high‑dose chemotherapy, which can cause:
- Transient neutropenia leading to infection.
- Cardiac or pulmonary toxicity (rare with modern regimens).
- Secondary malignancies - long‑term surveillance is advised.
MSC therapy’s side‑effect profile is milder, typically limited to fever, headache, or mild rash after infusion. Nonetheless, both therapies require regular MRI scans (every 3‑6 months) and neurologic exams to track disease trajectory.
Future Directions and Emerging Research
Several Phase III trials are underway in 2025 to answer lingering questions:
- MSC‑PROGRESS - a multinational study evaluating repeated MSC infusions combined with low‑dose natalizumab.
- STAR‑SPMS - compares autologous HSCT against a next‑generation oral DMT (siponimod) in patients with active SPMS.
- Gene‑edited induced pluripotent stem cells (iPSCs) are being explored to deliver personalized neuroprotective factors directly into the CNS.
Early data suggest that combining immune reset (HSCT) with neuroprotective MSCs could produce additive benefits, a hypothesis that many academic centers are testing in pilot studies.
Bottom Line
For patients with active SPMS, stem cell therapy offers a compelling alternative to the status‑quo. HSCT delivers the biggest impact but requires careful patient selection and a seasoned transplant team. MSCs provide a lower‑risk option, especially for those who cannot tolerate intensive conditioning. As trial results continue to pour in, clinicians are likely to refine algorithms that match the right cell‑type to each patient’s disease profile.
What is the difference between HSCT and MSC therapy?
HSCT uses high‑dose chemotherapy to wipe out the existing immune system and then re‑infuses the patient’s own hematopoietic stem cells, essentially resetting immunity. MSC therapy injects multipotent stromal cells that modulate inflammation and release growth factors without the need for chemotherapy.
Who is eligible for stem cell therapy in SPMS?
Eligibility typically requires documented disease activity in the past 12 months, an Expanded Disability Status Scale (EDSS) score of 6.5 or lower, and adequate organ function to tolerate conditioning. A thorough cardiac, pulmonary, and infection work‑up is also mandatory.
How long does the HSCT procedure take?
The entire process, from stem‑cell mobilization to hospital discharge after conditioning, usually spans 2‑3 weeks. Recovery and immune reconstitution may take another 4‑6 weeks before the patient regains full blood counts.
Are there any long‑term risks after stem cell therapy?
For HSCT, concerns include secondary malignancies and organ toxicity that can appear years later. MSC therapy has a favorable safety record, but long‑term efficacy data are still limited, so ongoing monitoring is advised.
Can stem cell therapy be combined with standard DMTs?
Yes, many protocols begin with HSCT to reset immunity and then introduce a low‑risk DMT for maintenance. Ongoing trials are also testing MSC infusions alongside oral agents to see if synergistic effects improve neuroprotection.

hema khatri
Wow, this stem‑cell breakthrough is truly amazing!!! It feels like our country finally gets the recognition it deserves for pioneering such advanced therapies!!! The science behind resetting the immune system is solid, and the results speak for themselves. I’m thrilled that patients with active SPMS now have a real chance at improved quality of life!!!
Jennell Vandermolen
Thanks for sharing, it’s helpful to see the data laid out clearly.
Mike Peuerböck
The advent of autologous hematopoietic stem cell transplantation represents a paradigm shift in the therapeutic armamentarium for secondary progressive multiple sclerosis. By employing high‑dose immuno‑ablative conditioning followed by reinfusion of CD34‑positive progenitors, clinicians aim to eradicate autoreactive lymphocytes. Numerous phase‑II investigations have demonstrated a pronounced reduction in annualized relapse rates, frequently surpassing the 70 % threshold. Moreover, longitudinal follow‑up has revealed modest but statistically significant improvements in Expanded Disability Status Scale scores. Such functional gains, albeit limited to a subset of patients with relatively preserved ambulatory capacity, underscore the potential for disease modification. The safety profile of contemporary protocols has been refined through meticulous patient selection and supportive care measures. Mortality associated with transplantation now resides below one percent in high‑volume centers, a testament to evolved conditioning regimens. Nevertheless, non‑lethal complications, including opportunistic infections and organ toxicities, persist and necessitate vigilant monitoring. Mesenchymal stem cell infusions, while ostensibly less invasive, furnish a distinct mechanistic avenue predicated upon immunomodulation and trophic factor secretion. The secretome of these multipotent stromal cells can attenuate pro‑inflammatory cytokine cascades and promote neuro‑axonal repair. Clinical trials evaluating repeated intravenous administrations have reported reductions in new magnetic resonance imaging lesions and amelioration of fatigue. However, the magnitude of clinical benefit remains inferior to that observed with hematopoietic stem cell transplantation, reflecting divergent therapeutic objectives. When juxtaposing these cellular approaches with conventional disease‑modifying therapies, the superiority of relapse suppression is unmistakable. Yet, the durability of these effects over a decade horizon remains an open question, inviting ongoing registry analyses. In conclusion, stem‑cell–based interventions constitute a promising frontier, yet they demand careful patient stratification, multidisciplinary oversight, and transparent communication of risks versus rewards.
Simon Waters
All that sounds great until you realize the pharma giants are funding these studies to push their own agendas.
Kajal Gupta
Hey folks, love seeing all the enthusiasm around stem‑cell options – it’s like watching science fiction become reality, yet the data still needs a solid peer review.
Zachary Blackwell
Honestly, the “real” story is that the elite labs are gatekeeping the technology, only releasing it to a privileged few while the rest of us are left guessing.
prithi mallick
i think its important to remember that every new treatment has its own risk and we should weigh them carefully before jumping into anything.
Michaela Dixon
Indeed, the intricate dance between immunological resetting and neuro‑protective strategies is fascinating; when we consider the cascade of cytokines that are modulated by mesenchymal cells, we enter a realm where biology meets art. The autologous HSCT protocol, with its rigorous conditioning phase, exemplifies a surgical precision that borders on alchemy. Moreover, the patient selection criteria-recent relapses, MRI activity, and an EDSS below 6.5-serve as a gatekeeper ensuring that only those most likely to benefit are exposed to the high‑intensity regimen. While the mortality rate has thankfully plummeted below one percent, the lingering specter of infection looms large, demanding a multidisciplinary supportive network. In parallel, MSC infusions, though less aggressive, whisper promises of trophic support, soothing inflammation subtly and safely. The modest reductions in lesion formation observed in phase II trials are encouraging, yet we must temper optimism with rigorous longitudinal data. Ultimately, the convergence of these therapies underscores a broader shift toward personalized medicine, where the nuances of each patient’s disease trajectory guide therapeutic choice.
James Gray
Super excited about these options – they could totally change the game for folks battling SPMS!
Scott Ring
I hear you, and it’s great to keep a balanced view while we wait for more long‑term results.
Shubhi Sahni
Fantastic overview!!! This really highlights how far we’ve come!!!
Danielle St. Marie
Well, if you’re not from a top-tier research nation, you’ll never see these breakthroughs – it’s a reality of global science 😡
Bonnie Lin
Interesting.