Cyclophosphamide vs. Alternatives Decision Guide
Drug Comparison Results
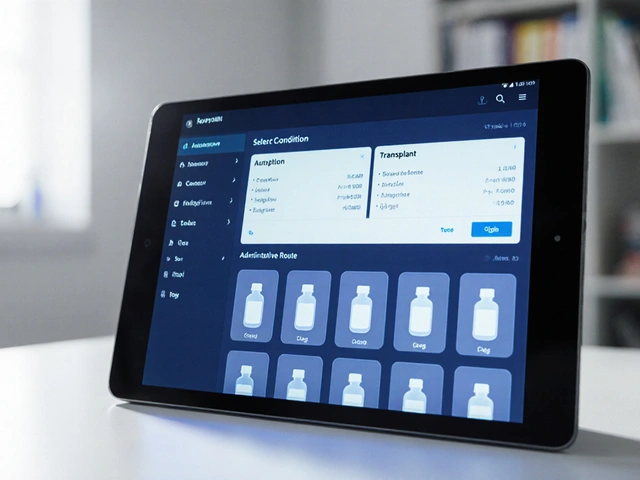
How to Use This Tool
Select a condition and administration route to see how cyclophosphamide compares with its alternatives.
- Autoimmune Disorders: Ideal for severe cases requiring strong immunosuppression
- Cancer Treatment: Effective for lymphomas, leukemias, and solid tumors
- Bone Marrow Transplant: Used for myeloablative conditioning regimens
Quick Summary
- Cytoxan (cyclophosphamide) is a versatile alkylating agent used for many cancers and autoimmune disorders.
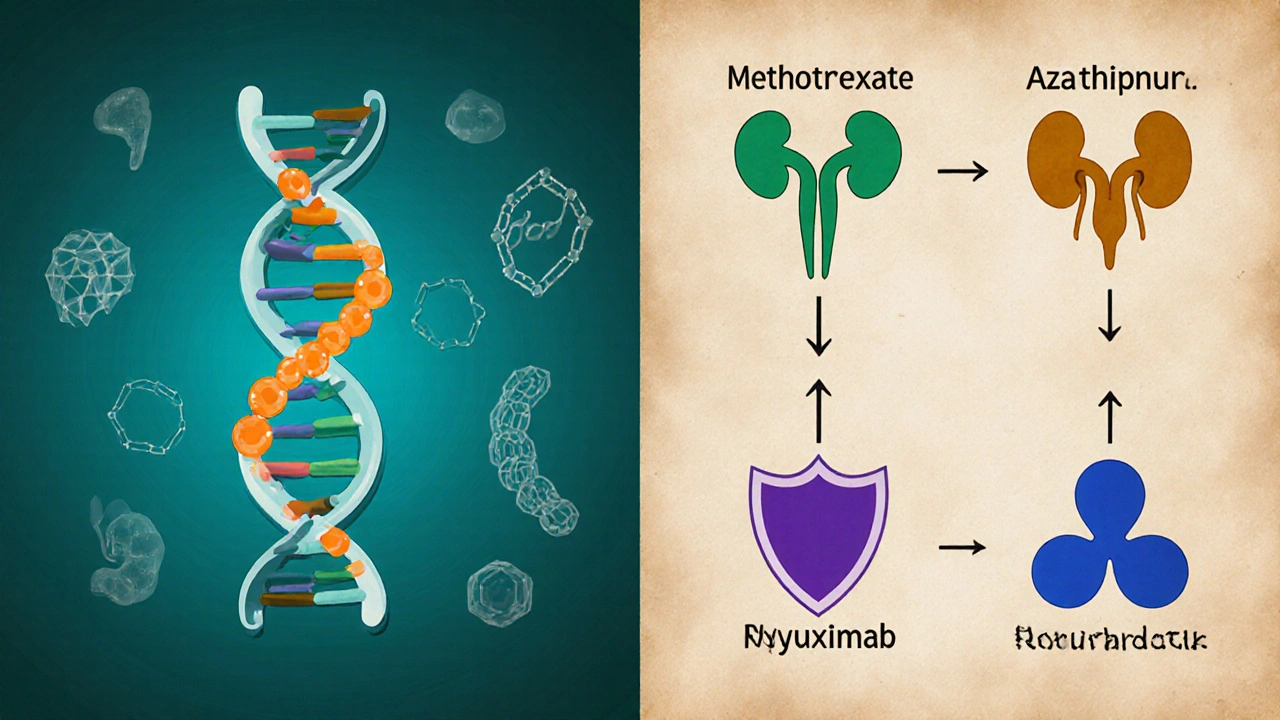
- Key alternatives include methotrexate, azathioprine, mycophenolate mofetil, rituximab, ifosfamide, chlorambucil and busulfan.
- Choosing the right drug depends on disease type, administration route, side‑effect profile and patient comorbidities.
- Oral drugs (e.g., methotrexate) are convenient for long‑term autoimmune therapy, while IV agents (e.g., rituximab) suit aggressive lymphomas.
- Close monitoring of blood counts and organ function is essential for all options.
What Is Cyclophosphamide?
Cyclophosphamide is a synthetic nitrogen mustard that works as an alkylating chemotherapy agent. It interferes with DNA replication, leading to cell death in rapidly dividing cells. Marketed under the brand name Cytoxan, it has been a backbone of oncology and rheumatology for decades.
How Cyclophosphamide Works
After oral ingestion or IV infusion, cyclophosphamide is metabolized in the liver to active compounds like phosphoramide mustard. These metabolites form cross‑links between DNA strands, preventing the cancer cell from copying its genetic material. In autoimmune disease, the same DNA damage dampens overactive immune cells, reducing inflammation.
Main Clinical Uses
Doctors prescribe cyclophosphamide for:
- Hematologic cancers such as non‑Hodgkin lymphoma, chronic lymphocytic leukemia and multiple myeloma.
- Solid tumours including breast, ovarian and lung cancer when combined with other agents.
- Autoimmune conditions like systemic lupus erythematosus, vasculitis and severe rheumatoid arthritis.
- Bone‑marrow transplant conditioning regimens.
Its flexibility comes from multiple dosing schedules-high‑dose IV pulses for aggressive disease or low‑dose oral long‑term regimens for autoimmune control.
Common Alternatives Overview
When cyclophosphamide isn’t ideal, clinicians turn to other drugs that hit similar pathways or target the same diseases.
Methotrexate is a folate antagonist that blocks DNA synthesis, widely used in low‑dose oral form for rheumatoid arthritis and psoriasis, and in high‑dose IV regimens for certain leukemias.
Azathioprine is a purine analog that reduces lymphocyte proliferation, often chosen for organ transplant maintenance and chronic autoimmune disorders.
Mycophenolate mofetil inhibits inosine monophosphate dehydrogenase, curbing B‑ and T‑cell growth; it’s popular in lupus nephritis and transplant prophylaxis.
Rituximab is a monoclonal antibody that depletes CD20‑positive B cells, effective for B‑cell lymphomas and refractory autoimmune disease.
Ifosfamide is a structural analog of cyclophosphamide used mainly for sarcoma and germ‑cell tumors, delivering similar alkylating activity but with a different toxicity pattern.
Chlorambucil belongs to the same alkylating family, historically used for chronic lymphocytic leukemia and low‑grade lymphomas.
Busulfan is a bifunctional alkylating agent employed in myeloablative regimens before bone‑marrow transplant.
Side‑Effect Profiles at a Glance
All these drugs affect rapidly dividing cells, so overlapping toxicities exist, but each has unique nuances.
- Cyclophosphamide: hemorrhagic cystitis, alopecia, myelosuppression, secondary malignancies.
- Methotrexate: liver fibrosis, mucositis, pulmonary toxicity.
- Azathioprine: bone‑marrow suppression, hepatotoxicity, increased infection risk.
- Mycophenolate mofetil: gastrointestinal upset, leukopenia, teratogenicity.
- Rituximab: infusion reactions, hepatitis B reactivation, progressive multifocal leukoencephalopathy (rare).
- Ifosfamide: neurotoxicity, renal tubular acidosis, hemorrhagic cystitis (similar to cyclophosphamide).
- Chlorambucil: prolonged myelosuppression, secondary cancers.
- Busulfan: pulmonary fibrosis, seizures (requires anticonvulsant prophylaxis).
Comparison Table
| Drug | Primary Indications | Route & Typical Dose | Major Side‑Effects | Notable Advantage |
|---|---|---|---|---|
| Cyclophosphamide | Cancers (lymphoma, breast), severe autoimmune disease | IV 500‑1000mg/m² pulse or PO 1‑2mg/kg daily | Hemorrhagic cystitis, infertility, leukopenia | Broad spectrum-works for both oncology and rheumatology |
| Methotrexate | Rheumatoid arthritis, psoriasis, certain leukemias | PO 7.5‑25mg weekly or IV 1‑3g/m² high‑dose | Liver toxicity, mucositis, pulmonary fibrosis | Oral weekly dosing makes long‑term use convenient |
| Azathioprine | Transplant maintenance, inflammatory bowel disease | PO 1‑3mg/kg daily | Bone‑marrow suppression, hepatotoxicity | Relatively inexpensive generic option |
| Mycophenolate mofetil | Lupus nephritis, transplant prophylaxis | PO 1‑1.5g twice daily | GI upset, leukopenia, teratogenic | Less hepatotoxic than azathioprine |
| Rituximab | B‑cell lymphoma, refractory rheumatoid arthritis | IV 375mg/m² weekly ×4 or every 6months | Infusion reactions, infection risk, rare PML | Targets B‑cells directly, sparing other immune cells |
| Ifosfamide | Sarcoma, germ‑cell tumors | IV 1.2‑1.8g/m² daily ×3‑5 days | Neurotoxicity, renal tubular acidosis, cystitis | Effective in tumors resistant to cyclophosphamide |
| Chlorambucil | Chronic lymphocytic leukemia, low‑grade lymphoma | PO 0.1‑0.2mg/kg daily | Myelosuppression, secondary malignancies | Oral administration, easy outpatient use |
| Busulfan | Myeloablative conditioning before transplant | IV 0.8‑1mg/kg hourly ×4‑6 doses | Pulmonary fibrosis, seizures | Potent myeloablation for stem‑cell rescue |
Decision‑Making Criteria
When you or your doctor weigh options, consider four practical questions:
- What disease am I treating? Some drugs (e.g., rituximab) excel in B‑cell lymphoma but add little for diffuse large‑B‑cell disease where cyclophosphamide already shines.
- Do I need oral convenience or can I tolerate IV infusions? Oral methotrexate and azathioprine spare clinic visits; IV cyclophosphamide or rituximab require scheduled appointments.
- How robust is my organ function? Pre‑existing kidney disease tips the scale away from ifosfamide and cyclophosphamide, which generate toxic metabolites cleared renally.
- What is my tolerance for specific side‑effects? Concern about infertility may push younger patients toward methotrexate or mycophenolate, while severe disease may justify cyclophosphamide despite its risks.
Balancing these factors yields a personalized regimen that maximizes efficacy while minimizing harm.
Practical Tips & Common Pitfalls
Hydration matters. For cyclophosphamide and ifosfamide, adequate fluid intake (≥2L/day) plus MESNA prophylaxis drastically cuts bladder toxicity.
Regular blood count monitoring is non‑negotiable. Schedule CBCs weekly during high‑dose pulses, then taper to monthly once stable.
Never mix certain drugs without specialist guidance. Combining azathioprine with allopurinol can cause severe bone‑marrow suppression; dose adjustments are mandatory.
Pregnancy considerations: Cyclophosphamide, methotrexate and mycophenolate are teratogenic. Effective contraception must be in place for women of child‑bearing age.
Watch for drug‑specific warnings. Rituximab requires hepatitis B screening before first infusion, and patients need prophylactic antivirals if they test positive.
Mini FAQ
Is cyclophosphamide more effective than methotrexate for lupus?
Cyclophosphamide is usually reserved for severe, organ‑threatening lupus (e.g., nephritis, CNS involvement) because it offers faster, stronger immunosuppression. Methotrexate works well for milder joint disease but may not halt rapid kidney damage.
Can I take azathioprine and cyclophosphamide together?
Combining two strong alkylating agents is generally avoided due to overlapping bone‑marrow toxicity. If a clinician adds azathioprine, they will lower the cyclophosphamide dose and monitor counts closely.
What protects the bladder from cyclophosphamide damage?
MESNA (sodium 2‑mercaptoethane sulfonate) binds the toxic metabolite acrolein, preventing it from irritating the bladder lining. It’s given intravenously or orally alongside each cyclophosphamide dose.
Why might a patient prefer rituximab over cyclophosphamide?
Rituximab targets B cells specifically, sparing many other immune cells, which can mean fewer infections and no risk of hemorrhagic cystitis. It’s also given less frequently (every 6‑12 months) once the disease is under control.
Is busulfan ever used instead of cyclophosphamide for conditioning?
Yes, some transplant protocols use busulfan (often combined with fludarabine) as an alternative myeloablative regimen, especially when avoiding cyclophosphamide‑related liver toxicity.
Bottom Line
Cytoxan remains a go‑to drug when you need a broad‑spectrum, high‑impact cytotoxic agent. However, a growing toolbox of oral and targeted therapies means many patients can avoid its harsher side‑effects. By matching disease specifics, administration preferences, and safety concerns, you can pick the alternative that delivers the right balance of power and tolerability.

Danielle Greco
Wow, this guide really paints a vibrant picture of cyclophosphamide’s role in both oncology and rheumatology 🌈. The way the pros and cons are laid out feels like a roadmap through a dense forest, guiding us toward the safest clearing. I especially love the emphasis on hydration and MESNA – it’s the kind of practical tip that can save a lot of trouble later. The comparison table is crisp and colorful, making the data pop like fireworks on a night sky. Overall, an excellent blend of science and user-friendly flair! 😊
Linda van der Weide
Reading through the side‑effect profiles, one can’t help but notice how each drug walks a delicate line between therapeutic benefit and potential harm. It’s a reminder that medicine often feels like a philosophical balancing act, weighing mortality against quality of life. The tone here stays friendly yet grounded, making the heavy topics approachable. I appreciate the concise bullet points that keep the information digestible. Thanks for the thorough overview.
Philippa Berry Smith
While the article appears comprehensive, I remain skeptical of the seemingly neutral stance on cyclophosphamide’s carcinogenic potential. Hidden agendas often downplay the long‑term secondary malignancy risk, nudging clinicians toward a drug that may cause future crises. The data on hemorrhagic cystitis, for instance, is presented without stressing the crucial role of prophylactic measures, which could be interpreted as negligence. It’s vital to interrogate the sources behind these claims; otherwise, we risk becoming unwitting pawns. The meticulous grammar hides a deeper conspiracy within the medical literature.
Joel Ouedraogo
Let’s cut to the chase: cyclophosphamide is a powerhouse, but wield it without discipline and you’ll drown in toxicity. The arguments for its broad-spectrum efficacy are strong, yet they must be weighed against the irreversible damage it can inflict on reproductive health. This is not a debate, it’s a call for strategic application-high‑dose pulses when the disease demands, low‑dose maintenance otherwise. Ignoring the nuances is a disservice to patients. Precision in dosing is the only philosophy that matters here.
Beth Lyon
i think the comparrison is good but some parts r a bit confusing. the table is helpful but a bit too dense for a quick read. also maybe add a little more about how to monitor blood counts. it would be nice if the tool had a reminder for mesna usage. overall nice effort but could be simplified a tad.
Nondumiso Sotsaka
Great job putting all this info together! 🌟 Remember, each patient’s journey is unique, so tailoring the regimen to their specific needs is key. If you’re unsure about dosing schedules, consider a step‑wise approach: start low, monitor labs, then adjust. Keep the communication open with your healthcare team; they’re your allies. 💪 Stay hopeful and keep seeking the best balance for safety and efficacy.
Ashley Allen
Good summary, very concise.
Brufsky Oxford
Philosophically speaking, the choice of a chemotherapeutic agent mirrors the ancient dilemma of hedonism versus asceticism – do we seek rapid, potent eradication of disease (the hedonist) or opt for a gentler, long‑term management (the ascetic)? The trade‑offs outlined here echo that timeless debate. 🌿 The inclusion of both oral and IV options reflects the spectrum of patient autonomy versus clinical control. Interesting to ponder how each path shapes the patient’s existential narrative.
Lisa Friedman
Honestly the guide covers all the bases, but i think they missed a beat on drug interactions. Many patients on azathioprine also take allopurinol, which can cause severe myelosuppression if dosing isn’t adjusted. Also the mention of mesna is good, but don’t forget to advise patients to stay well hydrated to reduce bladder toxicity. The table is great but could use a bit more color coding for quick visual scan. Overall, solid effort though a few details could be sharpened.
cris wasala
Hey folks, love how this post breaks down the options in a way that feels welcoming and positive. Remember that choosing a drug is a collaborative journey, and staying optimistic can really help patients get through tough treatments. Keep supporting each other and share any tips that made your experience smoother. Together we can make the scary side of chemo a bit brighter.
Tyler Johnson
When we step back and examine the therapeutic landscape of cyclophosphamide and its numerous alternatives, we must first acknowledge the sheer breadth of clinical scenarios it spans. From aggressive lymphomas demanding high‑dose intravenous pulses to chronic autoimmune diseases where low‑dose oral regimens are the mainstay, cyclophosphamide’s versatility is unparalleled. Yet this very versatility introduces layers of complexity that cannot be understated. The decision matrix must account for disease pathology, patient comorbidities, and the intricate side‑effect profiles inherent to each agent. Hydration status, for instance, is a pivotal factor for cyclophosphamide and ifosfamide, as inadequate fluid intake can precipitate severe hemorrhagic cystitis. Moreover, the specter of secondary malignancies looms large, compelling clinicians to weigh long‑term risks against immediate therapeutic gains. In contrast, methotrexate offers a more convenient oral regimen but brings its own challenges, such as hepatotoxicity and the need for diligent liver function monitoring. Azathioprine, while cost‑effective, demands genetic testing for TPMT deficiency to avoid catastrophic bone‑marrow suppression. Mycophenolate mofetil’s favorable hepatic profile makes it attractive for lupus nephritis, yet its teratogenic potential mandates strict contraception. Rituximab stands out as a targeted monoclonal antibody, sparing many off‑target effects but requiring pre‑infusion screening for hepatitis B and vigilant infection surveillance. Ifosfamide, structurally akin to cyclophosphamide, provides a vital option for sarcomas resistant to other alkylators, but neurotoxicity remains a significant hurdle. Chlorambucil’s oral convenience is balanced by its propensity for prolonged myelosuppression, making it suitable mostly for indolent hematologic malignancies. Busulfan, reserved for myeloablative conditioning, brings the risk of pulmonary fibrosis and seizures, necessitating prophylactic anticonvulsants and pulmonary function testing. The art of drug selection thus becomes a tapestry woven from pharmacodynamics, toxicity spectrums, patient lifestyle, and resource availability. Regular laboratory monitoring-CBCs, renal and hepatic panels-is indispensable across all regimens to catch adverse trends early. Patient education on signs of infection, bleeding, and organ dysfunction further empowers individuals to participate actively in their care. Ultimately, while cyclophosphamide remains a cornerstone for many high‑risk conditions, the expanding armamentarium of alternatives allows for personalized strategies that can mitigate side effects while preserving efficacy. The nuanced balance between aggressiveness and tolerability defines modern therapeutic decision‑making, and embracing this complexity leads to better outcomes for patients navigating these challenging diagnoses.
Annie Thompson
The sheer volume of information laid out in that massive paragraph is both awe‑inspiring and a little overwhelming, almost like staring at a kaleidoscope of drug data without a clear focal point. It feels as though the author tried to cram every possible nuance into a single breath, leaving the reader gasping for a pause. Yet, within that torrent, there are pearls of wisdom about hydration, MESNA, and the ever‑present risk of secondary cancers. The narrative style borders on poetic, blending clinical facts with existential musings, which can be both engaging and confusing. One can’t help but wonder if the density of sentences might cause readers to miss crucial safety warnings hidden amid the flow. Still, the commitment to thoroughness is commendable, and the emphasis on monitoring labs is a vital reminder we often overlook. The balance between aggressive treatment and patient quality of life shines through as a central theme, echoing the age‑old battle between cure and comfort. All in all, a monumental effort that invites both admiration and a desire for a more digestible format.
Parth Gohil
From a pharmacological perspective, the integration of jargon such as "alkylating agent" and "bifunctional" serves to delineate mechanistic pathways, which is essential for clinicians seeking to align therapeutic strategy with molecular targets. The comparative analysis effectively highlights the kinetic profiles of intravenous versus oral bioavailability, thereby informing dosage titration decisions. It’s also noteworthy that the table leverages standardized metrics like mg/m², which facilitates cross‑study comparisons. Overall, the data architecture adheres to evidence‑based standards, providing a robust framework for decision support. The inclusion of side‑effect taxonomy further enhances clinical applicability.
VAISHAKH Chandran
Honestly the guide feels like it’s trying too hard to be inclusive while ignoring the core issues that matter most to our patients. Cyclophosphamide’s dominance is backed by decades of research, yet the narrative pushes newer drugs as if they’re universally superior. It’s a blatant attempt to rewrite history in favor of pharma’s marketing agendas. We must stay vigilant and not be swayed by superficial glamour.
Pat Merrill
Sure, the article is thorough, but let’s not pretend it’s a flawless masterpiece – a few spots read like a textbook copy‑paste session. The sarcastic undertone about “one‑size‑fits‑all” regimens is apt, yet the author could’ve cut the fluff. Still, credit for ditching the jargon in the summary; it makes the content more digestible for the layperson. Just wish there were more real‑world anecdotes sprinkled in. Overall, decent but not groundbreaking.
Vicki Roth
Interesting read, especially the part about monitoring blood counts regularly. It’s good to see a balanced take on both oral and IV options. I think the practical tips on hydration and MESNA are useful for patients. The tone stays casual yet informative, which helps keep the content approachable.
Vishal Bhosale
I think the guide could be better. Some points are oversimplified and ignore real costs. Not all patients can afford the newer drugs.
Garima Gauttam
Actually the cheaper options work just fine for many cases. Simpler is often better.