What’s Really Going On When Your Stomach Acts Up?
You eat a slice of pizza, and within an hour, your stomach starts cramping. Or maybe you drink a glass of milk and feel bloated all afternoon. Could it be a food allergy? Or just an intolerance? The difference matters-food allergy can kill. Food intolerance won’t. But both feel awful. And most people can’t tell them apart.
Let’s cut through the noise. If your gut is upset after eating, you’re not alone. About 1 in 5 Americans say they have a food intolerance. Only about 1 in 20 have a diagnosed food allergy. But here’s the problem: nearly 80% of people who think they have a food intolerance are wrong. Their symptoms? Actually caused by IBS, acid reflux, or celiac disease. Misdiagnosis is common. And the wrong guess can lead to unnecessary diets, stress, or even dangerous delays in treatment.
Food Allergy: Your Immune System Sounds the Alarm
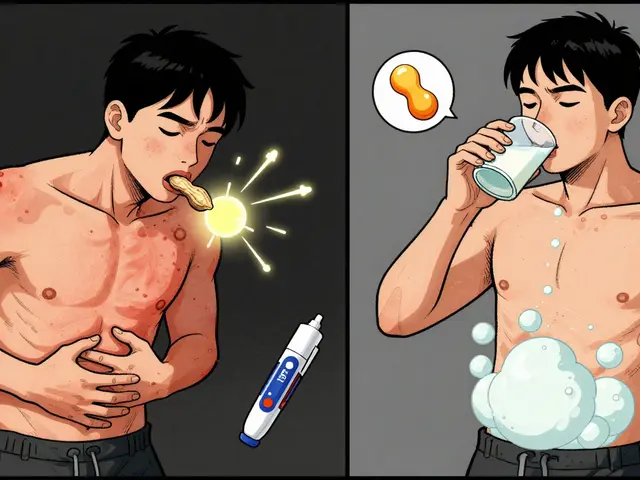
A food allergy isn’t just a bad reaction. It’s your immune system mistaking a harmless protein for a threat. That’s it. The body makes IgE antibodies to fight it. Those antibodies trigger mast cells to dump histamine and other chemicals into your bloodstream. Within minutes, you might get hives, swelling, vomiting, or trouble breathing. In severe cases, it’s anaphylaxis-your blood pressure drops, your airways close. Without epinephrine, it can be fatal.
The big eight allergens? Peanuts, tree nuts, milk, eggs, wheat, soy, fish, and shellfish. These cause 90% of reactions in the U.S. Even a tiny crumb can trigger a response. That’s why people with allergies carry EpiPens. That’s why labels say “may contain peanuts.” That’s why schools ban peanut butter. There’s no safe amount.
GI symptoms from a food allergy? They’re fast and loud. Vomiting. Severe abdominal pain. Diarrhea. But they don’t show up alone. You’ll usually also have skin reactions, swelling, or breathing issues. If your only symptom is bloating after eating beans? That’s not an allergy. That’s something else.
Food Intolerance: Your Gut Just Can’t Handle It
Food intolerance? No immune system involved. No antibodies. No anaphylaxis. It’s a digestive problem. Your body lacks the right enzyme to break something down. Or it’s sensitive to a chemical in the food. Lactose intolerance is the classic example. You don’t make enough lactase, so the lactose in milk travels undigested to your colon. Bacteria ferment it. Gas. Bloating. Cramps. Diarrhea. Symptoms show up 30 minutes to 2 hours later. And here’s the kicker: you can often handle a little bit. Most people with lactose intolerance can drink up to 1 cup of milk without trouble.
Other common intolerances? Fructose (in fruit and honey), histamine (in aged cheese, wine, cured meats), and sulfites (in dried fruit, wine, processed potatoes). Gluten intolerance? That’s tricky. Celiac disease is an autoimmune disorder triggered by gluten-it’s not an allergy, but it’s serious. Non-celiac gluten sensitivity is real too, but harder to diagnose. It doesn’t damage your gut like celiac, but it can cause bloating, fatigue, and brain fog.
Unlike allergies, intolerances don’t cause swelling, hives, or breathing problems. If you’re having those, it’s not just an intolerance. Get checked.
Testing for Allergies: What Actually Works
If you suspect a food allergy, see an allergist. Don’t rely on at-home kits or online tests. The only reliable methods are:
- Skin prick test: A tiny drop of allergen is placed on your skin, then lightly pricked. A raised bump (wheal) larger than 3mm means a likely allergy.
- Specific IgE blood test: Measures antibody levels. A result above 0.35 kU/L suggests allergy, but it’s not perfect-false positives happen.
- Oral food challenge: The gold standard. You eat increasing amounts of the food under medical supervision. If you react, you know for sure. This is the only way to confirm a diagnosis when tests are unclear.
Advanced tests like component-resolved diagnostics can tell you exactly which protein you’re allergic to. For example, Ara h 2 in peanuts is linked to severe reactions. If your test shows high levels, you’re at higher risk. This helps avoid unnecessary avoidance of foods that might be safe.
But here’s the red flag: IgG blood tests for “food sensitivities.” They’re everywhere online. They claim to find hidden allergies. They don’t. The American Academy of Allergy, Asthma & Immunology says they’re meaningless. Sensitivity rates? Below 30%. Specificity? Under 45%. They’re a waste of money-and can lead to dangerous food restrictions.

Testing for Intolerances: No Magic Bullet
There’s no single blood test for most food intolerances. Diagnosis is detective work.
- Lactose intolerance: Hydrogen breath test. You drink a lactose solution. Your breath is tested for hydrogen. A rise of 20 ppm above baseline means malabsorption.
- Celiac disease: Blood test for tissue transglutaminase antibodies (tTG-IgA). If it’s over 10 U/mL, you need a biopsy. The biopsy shows damage to your small intestine-Marsh 3 classification confirms it.
- Non-celiac gluten sensitivity: No test exists. You must eliminate gluten for 2-6 weeks, then reintroduce it. If symptoms return, it’s likely the culprit. But only after ruling out celiac and wheat allergy.
- Fructose or FODMAP intolerances: Elimination diet followed by challenge. Work with a dietitian. The low-FODMAP diet is proven to help IBS and many food intolerances.
Important: Don’t skip testing for celiac before going gluten-free. If you cut out gluten first, the blood tests and biopsy won’t show anything. You’ll never get a real diagnosis.
What Happens If You Get It Wrong?
Thinking you have a food allergy when you don’t? You might avoid nutritious foods for no reason. Milk, eggs, wheat-these are important. Unnecessary avoidance can lead to nutrient gaps, especially in kids.
Thinking you have an intolerance when you actually have a food allergy? That’s dangerous. You might eat a small amount of peanut or shellfish, thinking it’s “safe,” and end up in the ER.
And if you ignore real conditions like celiac disease or IBS? Long-term damage can happen. Untreated celiac leads to osteoporosis, infertility, even intestinal cancer. IBS left unmanaged affects your quality of life for years.
One 2023 study found that 45% of people who thought they had a food intolerance actually had IBS. Another 12% had inflammatory bowel disease. Both need different treatment than dietary tweaks.
Management: Avoidance vs. Moderation
With a food allergy: total avoidance. Always. Labels matter. Cross-contamination matters. Carry epinephrine. Even if your last reaction was mild, the next one could be worse. There’s no safe bet.
With a food intolerance: it’s about finding your threshold. You don’t have to give up everything.
- Lactose intolerance? Try lactose-free milk. Or take lactase pills before dairy. Hard cheeses and yogurt often have less lactose and are better tolerated.
- Sulfite sensitivity? Avoid wine, dried fruit, and pre-cut potatoes. Check ingredient lists for sulfites (E220-E228).
- Gluten sensitivity? Gluten-free oats, rice, quinoa, and vegetables are safe. Avoid wheat, barley, rye.
Many people with intolerances can eat small amounts without symptoms. That’s the big difference from allergies. You’re not allergic to life-you’re just sensitive to a specific food component.

When to See a Doctor
See a doctor if:
- You have vomiting, diarrhea, or abdominal pain after eating, especially if it’s recurring.
- You have skin reactions, swelling, or trouble breathing with any food.
- You’ve eliminated foods on your own and feel worse or more restricted.
- You’ve been told you have a “food sensitivity” based on an IgG test.
- You’re losing weight, have blood in your stool, or have persistent fatigue.
Don’t self-diagnose. Don’t trust online tests. Go to a gastroenterologist or allergist. Get the right tests. Get the right answer.
What’s New in 2026?
Research is moving fast. In 2024, scientists identified specific blood metabolites that distinguish non-celiac gluten sensitivity from IBS with 89% accuracy. That’s huge. Soon, we might have a blood test for it.
Basophil activation tests and component-resolved diagnostics are becoming more common in clinics. These help predict severity before a reaction even happens.
FARE (Food Allergy Research & Education) is funding 17 active clinical trials. The goal? Better testing. Better treatments. And for the first time, real hope for people who live in fear of their next meal.
Can you outgrow a food allergy?
Yes, some children outgrow allergies to milk, eggs, wheat, and soy-often by age 10. Peanut, tree nut, fish, and shellfish allergies are usually lifelong. Only about 20% of peanut-allergic children outgrow it. Testing should be done under medical supervision, never at home.
Is celiac disease the same as a wheat allergy?
No. A wheat allergy is an IgE-mediated immune reaction to wheat proteins. It can cause hives, vomiting, or anaphylaxis. Celiac disease is an autoimmune disorder where gluten damages the small intestine. Symptoms are mostly GI but also include fatigue and anemia. They’re diagnosed differently and managed differently. You can have one, both, or neither.
Can stress make food intolerance worse?
Absolutely. Stress affects your gut-brain axis. It can slow digestion, increase inflammation, and make you more sensitive to FODMAPs or other triggers. Many people notice worse bloating or cramps during high-stress periods. Managing stress with sleep, exercise, or mindfulness can help reduce symptoms-even if you’re still eating the same foods.
Do probiotics help with food intolerances?
Some strains show promise. For lactose intolerance, certain probiotics like Lactobacillus acidophilus can help break down lactose in the gut. For IBS, Bifidobacterium infantis has been shown to reduce bloating. But probiotics aren’t a cure. They’re a support tool. Results vary by person. Don’t expect miracles.
Why do some people react to foods they’ve eaten for years?
Your body changes. Enzyme production can drop with age-lactase levels naturally decline after childhood. Gut bacteria shift. Stress, antibiotics, or illness can damage your gut lining. A food you tolerated for decades might suddenly cause issues. It’s not a new allergy. It’s your body’s capacity changing.
Final Takeaway
Food allergy = immune system. Fast. Dangerous. Needs epinephrine. Food intolerance = digestive system. Slower. uncomfortable. Usually manageable. Don’t guess. Get tested. Know what you’re dealing with. Your gut-and your life-depend on it.


Write a comment