Every year, hundreds of thousands of people end up in the hospital because of dangerous drug combinations. Many of these cases could have been avoided with a simple tool: a drug interaction checker. Whether you're taking a prescription, an over-the-counter pill, or a supplement, your meds don’t exist in isolation. They talk to each other - sometimes helpfully, sometimes dangerously. Knowing how to use a drug interaction checker isn’t just smart; it’s a basic part of staying safe.
What Is a Drug Interaction Checker?
A drug interaction checker is a digital tool that scans your list of medications and flags combinations that could cause harm. It doesn’t guess. It uses real pharmacology data to tell you if mixing, say, warfarin and ibuprofen could lead to bleeding, or if taking statins with grapefruit juice might damage your liver. These tools are used by doctors, pharmacists, and patients alike. Some are built into hospital systems like Epic or Cerner. Others live in apps like Medisafe or on websites like the University of Liverpool’s DDI Checker.The science behind them is solid. They pull from databases that track thousands of documented interactions - from mild stomach upset to life-threatening heart rhythm problems. The best ones even account for how you take the drug: oral vs. injection, daily dose vs. occasional use, or even your age and kidney function in advanced versions.
Why You Need One - Even If You’re Healthy
You might think, “I only take one or two meds. I’m fine.” But here’s the catch: most people don’t realize how many substances they’re actually using. Think about it:- Your daily aspirin
- The ibuprofen you take for back pain
- The melatonin for sleep
- The St. John’s Wort for mood
- The calcium supplement from the health food store
That’s five items. Now add your prescription blood pressure pill. That’s six. And you didn’t even mention your tea or grapefruit juice. According to the CDC, nearly half of U.S. adults take at least one prescription drug. One in four take five or more. And 80% of those people also use supplements or OTC meds. The risk isn’t theoretical - it’s statistical.
A 2022 study by the Agency for Healthcare Research and Quality found that drug interactions cause over 1.5 million preventable adverse events in U.S. hospitals every year. That’s more than car accidents. And most of those events happen because someone didn’t check.
How to Use a Drug Interaction Checker: A Simple 5-Step Process
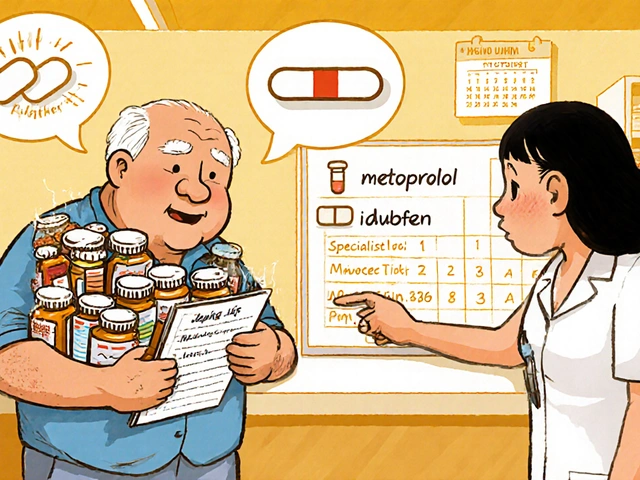
Using a drug interaction checker isn’t complicated. Here’s how to do it right, no matter which tool you’re using.- Make a full list of everything you take. Don’t leave anything out. Include prescriptions, OTC painkillers, vitamins, herbal supplements, and even recreational substances like alcohol. Write down the exact names and dosages. If you’re unsure, check the bottle or call your pharmacy.
- Choose your tool. For most people, a free app like Medisafe or a trusted website like the University of Liverpool’s DDI Checker works fine. If you’re a healthcare provider, your hospital likely uses Micromedex or Lexi-Interact. Pick one that’s easy to use and updated regularly.
- Enter your medications one by one. Most tools let you type in the name. Start with your main prescription. Then add each other item. If the tool suggests a list of matches, pick the exact one you take - don’t just pick the first result. For example, “ibuprofen” could mean 200mg tablets or a topical gel. The route matters.
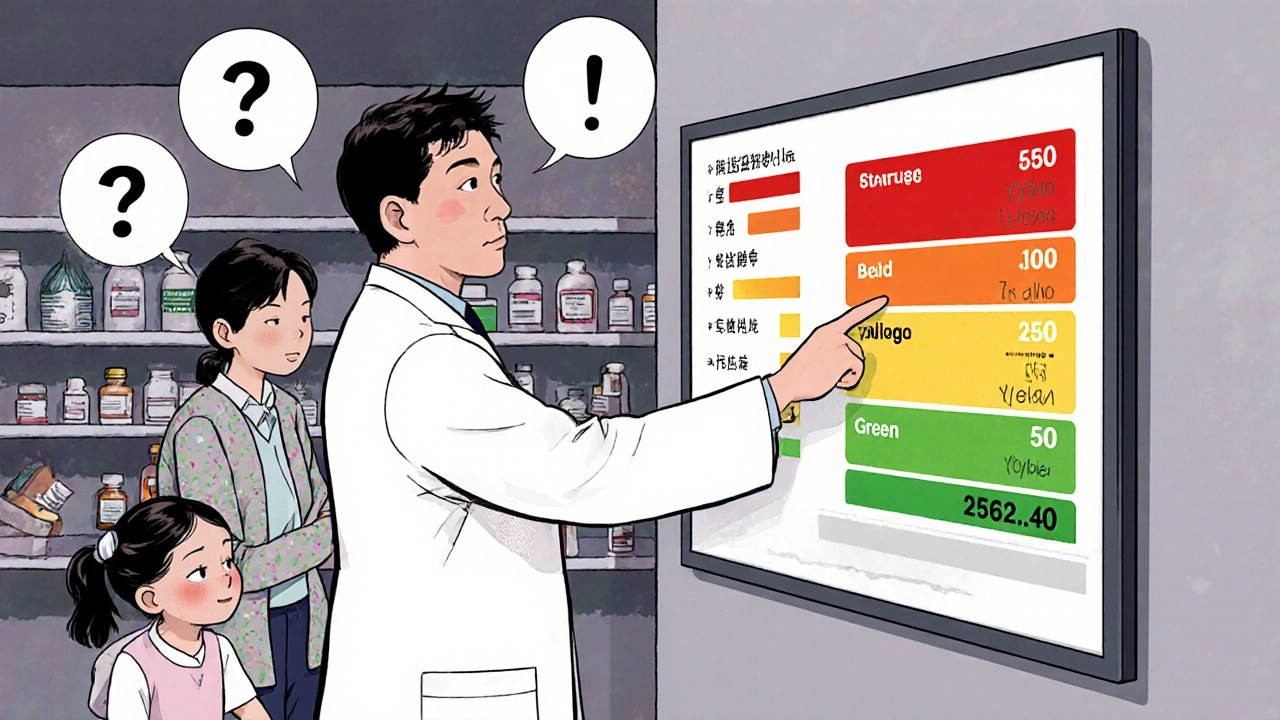
- Review the results carefully. Results are usually color-coded:
- Red = Dangerous. Don’t combine. Stop one or ask your doctor.
- Orange = Monitor closely. You might need a dose change or extra blood tests.
- Yellow = Minor. Note it, but no action needed.
- Green = No known interaction.
Click on any flagged interaction to read the explanation. It will tell you what happens - like “increased risk of bleeding” or “reduced effectiveness of the antibiotic.” Don’t skip this step.
- Take action. If you see a red alert, don’t ignore it. Call your doctor or pharmacist. Don’t stop your meds on your own - but do ask: “Is this combination safe? Is there a better option?” Keep a note of what you found and what you decided.
Top Tools You Can Use Right Now
You don’t need to buy anything. Here are the most reliable free and widely used options:| Tool | Type | Best For | Accuracy | Limitations |
|---|---|---|---|---|
| Medisafe (App) | Mobile app (iOS/Android) | Patients managing multiple meds | High - caught nearly 100,000 interactions since launch | Only shows interactions between drugs in its database; doesn’t track supplements well |
| University of Liverpool DDI Checker | Web-based | General use, including COVID-19 meds | Very high for viral treatments | Not designed for all drug classes - stick to its specialty |
| DrugBank | Web/API | Developers, researchers, advanced users | Excellent - includes supplements and food interactions | Requires technical knowledge; not user-friendly for casual users |
| Epocrates (App) | Mobile app | Healthcare professionals | High - 82% user satisfaction on speed | Only 63% of users trust its accuracy; some false positives |
| Lexi-Interact | Web/EHR integrated | Hospitals, clinics | Top-rated - highest accuracy score in NIH studies | Not free; requires institutional access |
For most people, start with Medisafe or the University of Liverpool’s checker. They’re free, easy, and reliable for everyday use.
What These Tools Can’t Do - And What You Must Do Instead
Here’s the hard truth: drug interaction checkers are powerful, but they’re not perfect. A 2022 review in JAMA Internal Medicine found that even the best systems miss 15% to 40% of dangerous interactions. Why?- They don’t know your full medical history - like if you have liver disease or are pregnant.
- They can’t tell if you’re taking a medication correctly - like if you crush pills or skip doses.
- They don’t understand your symptoms. If you’re dizzy, it might be the interaction - or something else.
- They often flag harmless combinations as “warnings,” leading to alert fatigue. One study found clinicians ignore nearly half of all alerts.
That’s why you must never rely on the tool alone. Always pair it with human advice. After you run your check:
- Bring the results to your pharmacist. They’re trained to interpret them.
- Ask your doctor: “Based on my health, is this combo safe for me?”
- If you’re on blood thinners, epilepsy meds, or heart drugs - never skip this step.
Pharmacists in the UK and US report that 68% of them use at least two interaction checkers daily - and still double-check manually. That’s not because they don’t trust tech. It’s because they know the stakes.
Common Mistakes People Make
Even when people use these tools, they often mess up. Here are the top five errors:- Only checking one new drug. You don’t just check the new pill you just got. You check it against everything you’re already taking.
- Using generic names incorrectly. Typing “aspirin” might not find “acetylsalicylic acid.” Use the exact name on the bottle.
- Ignoring supplements. St. John’s Wort, garlic pills, and ginkgo can interfere with antidepressants, blood thinners, and even anesthesia.
- Not updating the list. You stopped taking that antibiotic last month? Remove it. Old data = wrong results.
- Assuming “no interaction” means “safe for me”. Just because the tool says green doesn’t mean it’s right for your body. Your age, weight, and other conditions matter.
What Happens When You Don’t Use One
In 2021, a 72-year-old woman in Nottingham was admitted to hospital with internal bleeding. She’d been taking warfarin for atrial fibrillation and started taking ibuprofen for arthritis pain. She didn’t think it was a problem - “it’s just a painkiller.” The interaction wasn’t obvious to her. The drug interaction checker in her pharmacy’s system flagged it, but she never checked it herself.She survived. But she spent 11 days in the hospital. Her family paid thousands in medical bills. And she now has to take a different painkiller - one that’s less effective and more expensive.
This isn’t rare. It’s routine. Every day, someone makes the same mistake. You can avoid it.
Final Tips to Stay Safe
- Use a drug interaction checker every time you start, stop, or change a medication - even if it’s “just” a new vitamin.
- Keep a printed or digital list of all your meds and update it monthly.
- Ask your pharmacist to run a full interaction check during your next medication review.
- Don’t wait for a problem. Prevention is cheaper, safer, and less stressful.
- Teach a family member how to use the tool. If you’re ever unable to check yourself, they can help.
Medications save lives. But they can also hurt you - quietly, and without warning. A drug interaction checker is like a seatbelt for your health. It doesn’t guarantee safety, but it dramatically reduces the risk. And it takes less than five minutes.
Are drug interaction checkers accurate?
Yes, the best ones are highly accurate - especially Lexi-Interact and Micromedex, which scored top marks in NIH studies. But no tool is perfect. They miss about 15% to 40% of dangerous interactions, especially if your health conditions aren’t factored in. Always use them as a starting point, not the final answer.
Can I trust free apps like Medisafe?
Yes, for most people. Medisafe and similar apps use validated databases and are updated regularly. They’re excellent for personal use and catching common, serious interactions. But they don’t cover every supplement or rare drug combination. If you’re on complex meds (like for epilepsy or heart failure), always double-check with a pharmacist.
Do drug interaction checkers include supplements and herbal products?
Some do, some don’t. DrugBank and the University of Liverpool’s checker include many supplements. Medisafe and Epocrates are weaker here. If you take St. John’s Wort, garlic, ginkgo, or kava, make sure your tool lists them. If it doesn’t, assume the interaction might exist and ask a professional.
What should I do if a checker flags a red alert?
Don’t stop your medication suddenly. Call your doctor or pharmacist right away. Say: “My interaction checker flagged this combo as dangerous. Can we talk about alternatives?” Often, there’s a safer option - like switching from ibuprofen to acetaminophen, or changing the timing of doses.
Do hospitals use these tools?
Yes. Over 89% of U.S. hospitals use integrated systems like Micromedex or Lexi-Interact. They’re built into electronic health records and trigger alerts when a doctor prescribes a risky combo. But even then, clinicians override alerts 40% to 78% of the time - which is why patient involvement is critical.
Can I use these tools for my elderly parent?
Absolutely. Older adults are at the highest risk - they often take 5+ medications daily. Use Medisafe or the Liverpool checker together. Sit down with them, enter each pill, and review the results. Many families report it’s the first time their parent realized their “harmless” supplements were dangerous.
Next Steps to Take Today
If you’re reading this, you’re already ahead. Here’s what to do now:- Open your medicine cabinet. Write down every pill, capsule, patch, and supplement.
- Go to https://www.covid19-druginteractions.org/ (University of Liverpool’s free checker).
- Enter your list. One by one.
- Look at the results. If anything is red or orange, call your pharmacist tomorrow.
- Set a calendar reminder: check your meds again every 3 months.
It’s not about being paranoid. It’s about being informed. Your body is a system. Medications are tools. And tools only work safely when you understand how they interact. Use the checker. Talk to your pharmacist. Stay safe.



mohit passi
Just checked my meds on Medisafe and wow 🤯 turns out my turmeric + blood thinner combo is a red flag. I thought it was 'natural' so it was safe. Lesson learned. Thanks for the wake-up call.
Marissa Coratti
While I appreciate the thoroughness of this guide, I must emphasize that the reliance on digital tools without concurrent clinical consultation represents a dangerous paradigm shift in patient autonomy. The erosion of professional medical judgment in favor of algorithmic decision-making, however well-intentioned, undermines the very foundation of individualized care. One must consider not only pharmacokinetic interactions but also psychosocial context, adherence patterns, and the patient’s lived experience - factors that no database can quantify.
Micaela Yarman
I’m from the US and I’ve been telling my mom for years to check her supplements. She takes 12 things a day and swears ‘it’s all natural.’ Then she got hospitalized last year for a bleeding episode. Turns out, her ginkgo + aspirin was the culprit. This post? Needed. Share it with your grandma.
Amanda Wong
Let’s be real. These ‘interaction checkers’ are just marketing tools for Big Pharma. They flag everything to scare you into buying their branded alternatives. I’ve seen green flags turn red because a supplement had ‘citrus’ in the name - even though it was just a flavor additive. Don’t trust algorithms. Trust your doctor - if you have one.
james thomas
I’m not saying the tool is useless, but have you seen how many people just copy-paste their meds into Medisafe and then panic? I know a guy who stopped his antidepressant because it ‘interacted’ with his protein shake. Bro, that’s not an interaction - that’s just bad life choices. Also, why are we letting apps decide what we can take? Next they’ll tell us what to eat.
Deborah Williams
Oh wow, so now we’re outsourcing our medical decisions to free apps because we’re too lazy to read the tiny print on the bottle? How convenient. I’m sure the FDA is thrilled. Meanwhile, the real problem is that people think ‘natural’ means ‘safe’ - and then blame the tool when their liver fails. The tool didn’t lie. You did.
Kaushik Das
Man, this hits different coming from India where people mix ayurvedic stuff with Western meds like it’s a smoothie. My uncle took ashwagandha with his BP meds and ended up in the ER with a heart rate of 42. He thought it was ‘boosting his energy.’ I showed him the Liverpool checker and his face turned white. We need more of this - especially in places where pharmacy access is a bus ride away.
Asia Roveda
This is why America is collapsing. People think a phone app can replace decades of medical training. We’ve got folks Googling chemo alternatives and then blaming the system when they die. These checkers are fine for beginners - but if you’re on five meds and still trusting a free app, you’re one step away from a coroner’s report.
Aaron Whong
The epistemological framework underpinning these interaction checkers is fundamentally reductionist. Pharmacodynamics cannot be adequately modeled through binary flagging systems when ontological variability - i.e., individual phenotypic expression, gut microbiome modulation, and CYP450 polymorphisms - remains unaccounted for in consumer-facing interfaces. The green/red paradigm is a performative illusion of safety.
Sanjay Menon
I’ve used Lexi-Interact at work. It’s the gold standard. But I’ve also seen residents ignore 90% of the alerts because they’re ‘overwhelmed.’ So what’s the point? The system’s broken. We need AI that learns from real-world outcomes, not just static databases. And until then? This post is just another feel-good checklist for people who don’t want to pay for real care.
Cynthia Springer
I used the Liverpool checker and found out my vitamin D and thyroid med interact. I didn’t even know they were connected. I called my pharmacist and they said to take them 4 hours apart. Simple fix. I’m glad I checked. I didn’t need to be scared - just informed.