Every year, thousands of older adults in the UK end up in hospital because they’re taking two pills that do the same thing - and no one caught it. It’s not a mistake by a doctor. It’s not laziness. It’s a system gap. You see a cardiologist for your heart, a rheumatologist for your joints, and a neurologist for your nerves. Each one writes a prescription. None of them know what the others prescribed. And suddenly, you’re on two blood pressure meds, two statins, or two painkillers that should never be taken together. This isn’t rare. It’s duplicate medication - and it’s one of the most dangerous, yet preventable, problems for seniors on multiple drugs.
Why Duplicate Medications Happen
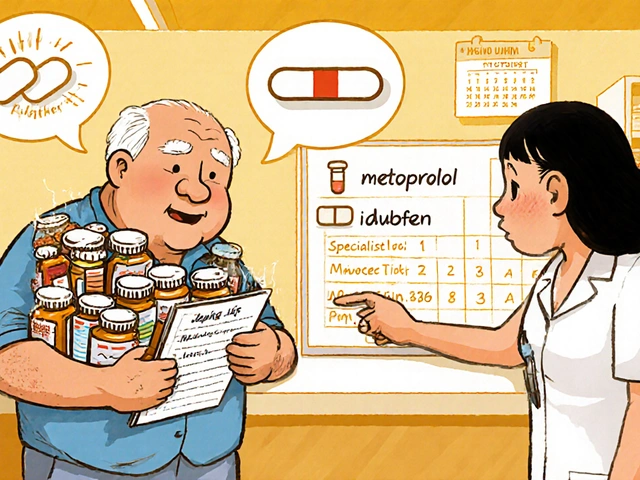
It’s not that doctors are careless. It’s that the system doesn’t talk to itself. Your GP might have a full list of your meds. But when you see a specialist, they often only see what’s in their own electronic record - not what you’re taking elsewhere. A 2015 study across 53 UK and US community pharmacies found that for every 100 prescriptions filled, over 20 triggered a duplicate medication alert. That’s one in five. And in nearly one-third of those cases, pharmacists had to take action - because the system missed it. The problem gets worse with age. The more conditions you have, the more specialists you see, and the more pills you take. Research shows that seniors on five or more medications are at the highest risk. A blood thinner like warfarin paired with an over-the-counter NSAID like ibuprofen? That’s a recipe for internal bleeding. Two beta-blockers? That can crash your heart rate. A statin and a fibrate together? That’s muscle damage waiting to happen. And here’s the kicker: many of these duplicates are never caught until someone ends up in A&E. A Reddit user shared how their dad was prescribed metoprolol by his cardiologist - unaware his GP had already prescribed it for high blood pressure. His pulse dropped to 42. He nearly had a fall. He didn’t know he was on two of the same drug until he checked his pill bottles.What You Can Do Right Now
You don’t need to wait for your doctor to fix this. You can stop it before it starts. Here’s exactly what to do.- Make a complete, up-to-date list of every medication you take. Not just prescriptions. Include over-the-counter painkillers, vitamins, herbal supplements, and even eye drops or creams. Write down the name, dose, and why you take it. Example: Atorvastatin 20mg - for high cholesterol.
- Bring your pill bottles to every appointment. Don’t rely on memory. A bottle says “Take one daily” - but your list says “Take two.” Which one’s right? Your pharmacist or doctor can check the label against your list and spot mismatches.
- Use one pharmacy for everything. This isn’t optional. If you use multiple pharmacies, none of them have your full history. One pharmacy sees your blood pressure meds. Another sees your diabetes pills. But only one pharmacy can see them all. That’s how they catch duplicates before you even leave the counter.
- Ask your pharmacist to review your list every time you pick up a new prescription. Pharmacists are trained to spot duplicates. They have tools that flag when two drugs are in the same class. Ask them: “Could any of these be doing the same thing?”
How to Talk to Your Doctors
Doctors aren’t mind readers. You have to speak up. Before every specialist visit, say this:“I’m on several medications. I want to make sure nothing I’m taking now is doing the same thing as what you’re prescribing. Can we go over my list together?”If they say yes, great. If they say no, bring your list anyway. Hand it to them. Say: “I’ve been told this helps avoid mistakes.” Most will accept it. And if they don’t? Ask to speak to their nurse or practice manager. You’re not being difficult - you’re protecting your life. Also, ask this question after any new prescription:
“Is this medicine replacing something I’m already taking - or adding to it?”If the answer is “adding,” ask: “Why can’t we stop the other one?” Sometimes, the answer is “We need both.” But often, it’s “We didn’t realize you were already on it.”
The Power of Medication Reconciliation
This isn’t just a buzzword. It’s a lifesaving process. Medication reconciliation means comparing what you’re supposed to be taking with what you’re actually taking - at every transition of care: when you leave hospital, when you see a new specialist, even when you switch GPs. The Joint Commission requires hospitals and clinics to do this. But in practice, it often doesn’t happen unless you push for it. After a specialist visit, ask your GP: “Can we do a full medication review? I saw Dr. Smith this week and they prescribed something new.” A 2021 study from Kaiser Permanente showed that when clinics made it mandatory for doctors to include the reason for each prescription - like “for atrial fibrillation” or “for osteoarthritis” - duplicate prescriptions dropped by 37%. Why? Because if a doctor sees you’re on metoprolol for hypertension, and they write another beta-blocker for angina, they’ll see the overlap and ask: “Do we really need both?”Technology Can Help - But Only If You Use It
There are apps now that let you scan your pill bottles with your phone and build a digital list. Some even sync with your pharmacy or GP system. The NHS has pilot programs using these tools in Nottingham and Manchester. They’re free. They’re easy. And they work. If you’re comfortable with your phone, try the NHS app. It lets you view your prescriptions and see what’s been issued. You can also download free apps like Medisafe or MyTherapy. They let you take photos of your pills, set reminders, and generate a printable list to bring to appointments. But don’t rely on tech alone. It’s a tool - not a replacement for your own vigilance. If your app says you’re on two statins, but your doctor says it’s fine, ask why. Get it in writing.
What to Do If You Already Have a Duplicate
If you suspect you’re taking two drugs that do the same thing - don’t stop either one on your own. That’s dangerous. Instead:- Write down both drug names and why you think they’re duplicates.
- Call your GP and say: “I think I might be on two medications that treat the same condition. Can we review them?”
- Bring your list and pill bottles to the appointment.
- Ask: “Which one should I keep? Can we stop the other one safely?”
Who to Call When Things Get Confusing
If you’re overwhelmed, reach out to your local NHS pharmacy. Many offer free “medicines use reviews” - a 20-minute chat with a pharmacist to go over everything you’re taking. No appointment needed in many areas. Just walk in. You can also call NHS 111 and ask: “I’m worried about duplicate medications. Can you connect me with a medicines safety advisor?” They’ll route you to the right person. And if you have a carer or family member helping you - include them. They can help track pills, remember questions to ask, and spot changes you might miss.Final Thought: You’re the Boss of Your Meds
No one cares more about your health than you do. Specialists focus on one part of you. Your GP tries to see the whole picture. But only you hold the full list - the bottles, the names, the doses, the reasons. You don’t need to be an expert. You just need to be prepared. Keep your list updated. Bring your bottles. Ask the questions. Use one pharmacy. Talk to your pharmacist. This isn’t about being difficult. It’s about being safe. And in the end, the people who avoid hospital visits after specialist visits aren’t the ones with the best doctors. They’re the ones who asked the questions.How do I know if I’m taking duplicate medications?
Look at your medication list. If two drugs have the same generic name - like metoprolol and metoprolol - or if they’re in the same class (e.g., two different ACE inhibitors), you may have a duplicate. Also check if two different brand names treat the same condition - like two blood pressure pills or two statins. Your pharmacist can quickly compare them using their system.
Can over-the-counter medicines cause duplicate prescriptions?
Absolutely. Many OTC painkillers like ibuprofen, naproxen, and diclofenac are NSAIDs - and if you’re already on a prescription NSAID, taking more can lead to stomach bleeding or kidney damage. Even common supplements like fish oil or garlic pills can thin your blood and interact with warfarin. Always include everything on your list.
Why can’t my doctors just share my records?
They can - but they don’t always. Different clinics use different systems. Your GP might use SystmOne, your cardiologist uses EMIS, and the hospital uses Epic. These systems don’t always talk to each other. Even when they do, specialists often don’t have full access to your primary care records unless you give permission. That’s why you need to bring your own list.
Is it safe to stop a duplicate medication on my own?
No. Stopping a medication suddenly - especially for blood pressure, heart conditions, or seizures - can be dangerous. Always talk to your GP first. They can help you taper off safely or switch to one better-suited drug. Never assume one pill is safer than another without professional advice.
How often should I update my medication list?
Update it every time you start, stop, or change a dose - even for a single pill. Also update it before every doctor or specialist appointment. Keep a printed copy in your wallet and a digital version on your phone. If you’re in an emergency, that list could save your life.
What if my pharmacist says a duplicate is okay?
Ask why. Sometimes, two drugs in the same class are used together intentionally - like low-dose aspirin with a statin for heart protection. But that’s rare. If your pharmacist says it’s safe, ask them to explain the reason in writing. If you’re still unsure, ask your GP for a second opinion. Trust your gut - if something feels off, it probably is.



Ady Young
I never realized how dangerous this was until my mom ended up in the ER after taking ibuprofen with her blood thinner. She didn’t even know it was a problem. Now she brings her pill bottles to every appointment and we update the list together. It’s a small habit, but it saved her life.
Don’t wait for a crisis. Start today.
Travis Freeman
This is such a needed post! I’ve been telling my dad for years to bring his meds to appointments, but he always says ‘I know what I’m taking.’ Spoiler: he doesn’t. Now I print out his list every time he sees a new doc. He still grumbles, but he hasn’t had any scary incidents since. Thanks for putting this out there - it’s the kind of info that doesn’t get talked about enough.
Keep spreading this stuff. We need more people like you.
Sean Slevin
Okay, so… here’s the thing: the system doesn’t talk to itself… but why? Why? WHY?!? Because of silos! Because of legacy tech! Because of $$$! Because no one’s incentivized to fix it! It’s not incompetence - it’s capitalism! We’ve got AI that can predict your next Netflix binge, but can’t sync your blood pressure meds across three different clinics? Come on!
And don’t even get me started on how the NHS and EMIS and SystmOne still don’t play nice… it’s like the digital equivalent of sending letters via carrier pigeon in 2024.
Meanwhile, the people paying the price? Us. The elderly. The over-medicated. The confused. The ones who can’t even remember if they took their pill at 8 or 10.
Someone needs to sue the vendors. Someone needs to burn the EHRs down and start over. Or… we keep doing what we’re doing. Which is… bring the bottles. Write the list. Ask the questions. And pray.
God help us all.
Chris Taylor
My grandma used to forget which pills were which - she’d mix up her statin with her thyroid med. I started labeling everything with colored tape. Blue for heart, green for thyroid, red for pain. She still uses it. Simple. Cheap. Works.
And yeah, one pharmacy. Always. Even if it’s farther away. Worth it.
Melissa Michaels
Medication reconciliation is a standard of care in accredited facilities, yet it remains inconsistently applied in outpatient settings. Patients must be empowered as active participants in their care. The responsibility should not rest solely on the individual to maintain exhaustive documentation. Systemic reform is required to ensure interoperability and mandatory cross-provider communication.
That said, the practical advice provided in this post is sound and should be widely disseminated.
Nathan Brown
I used to think this was just a UK problem. Then my cousin in Ohio got prescribed two different SSRIs at the same time. Same doctor, two different visits. No one noticed. He ended up in the psych ward. Not because he was suicidal - because he was serotonin overloaded.
It’s not just about pills. It’s about trust. We trust doctors to know what they’re doing. But they’re drowning in data and deadlines.
So we become the data. We become the bridge. We become the human firewall.
Bring the bottles. Write it down. Say it out loud.
And if they roll their eyes? Smile. And say ‘I just want to make sure I don’t die.’
They’ll listen.
:)
Matthew Stanford
One pharmacy. Always. This is the single most important thing you can do.
It’s not complicated. It’s not expensive. It’s not hard.
Do it.
Olivia Currie
OH MY GOD I JUST REALIZED MY DAD’S BEEN ON TWO BETA-BLOCKERS FOR SIX MONTHS AND NO ONE TOLD HIM?!?!?!
WHY IS NO ONE TALKING ABOUT THIS?!?!?
WHY ISN’T THIS ON THE NEWS?!?!?
I’M CALLING HIS GP RIGHT NOW.
THANK YOU. THANK YOU. THANK YOU.
THIS POST JUST SAVED A LIFE.
Curtis Ryan
so i tried one of them apps that scans your pills? it messed up my vitamins and thought my fish oil was a blood thinner??
so now i just take pics of the bottles and keep em in a folder on my phone
works better than the app lol
Rajiv Vyas
fake problem. big pharma wants you confused so you keep buying pills. they don't care if you take two of the same thing - they make more money. the real issue is the system is rigged. your 'pharmacist' is just a sales rep in a white coat. your 'doctor' gets kickbacks. you think you're saving yourself? you're just feeding the machine.
stop taking pills. eat turmeric. drink lemon water. your body knows better.
and if you're still on meds? you're already dead inside anyway.