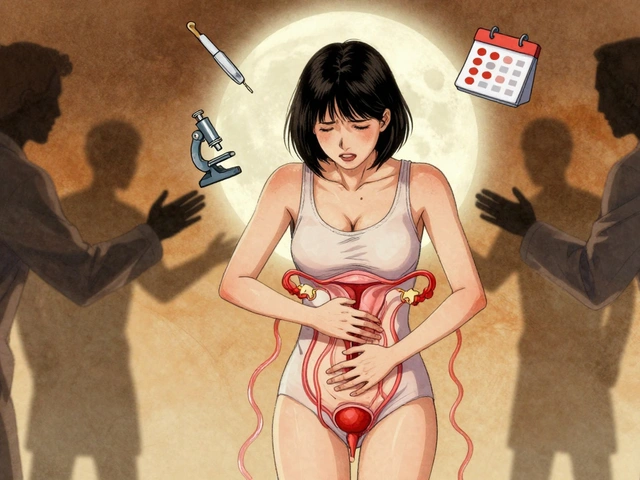
When you’ve been living with pelvic pain for months-or years-and every doctor tells you it’s just stress, or a UTI, or something you’ll grow out of, you start to wonder if it’s all in your head. It’s not. For millions of women, chronic pelvic pain isn’t a one-off issue. It’s two overlapping conditions hiding in plain sight: endometriosis and interstitial cystitis. They’re often called the ‘evil twins’ of pelvic pain because they look so similar, feel so similar, and get misdiagnosed so often.
What Exactly Is Endometriosis?
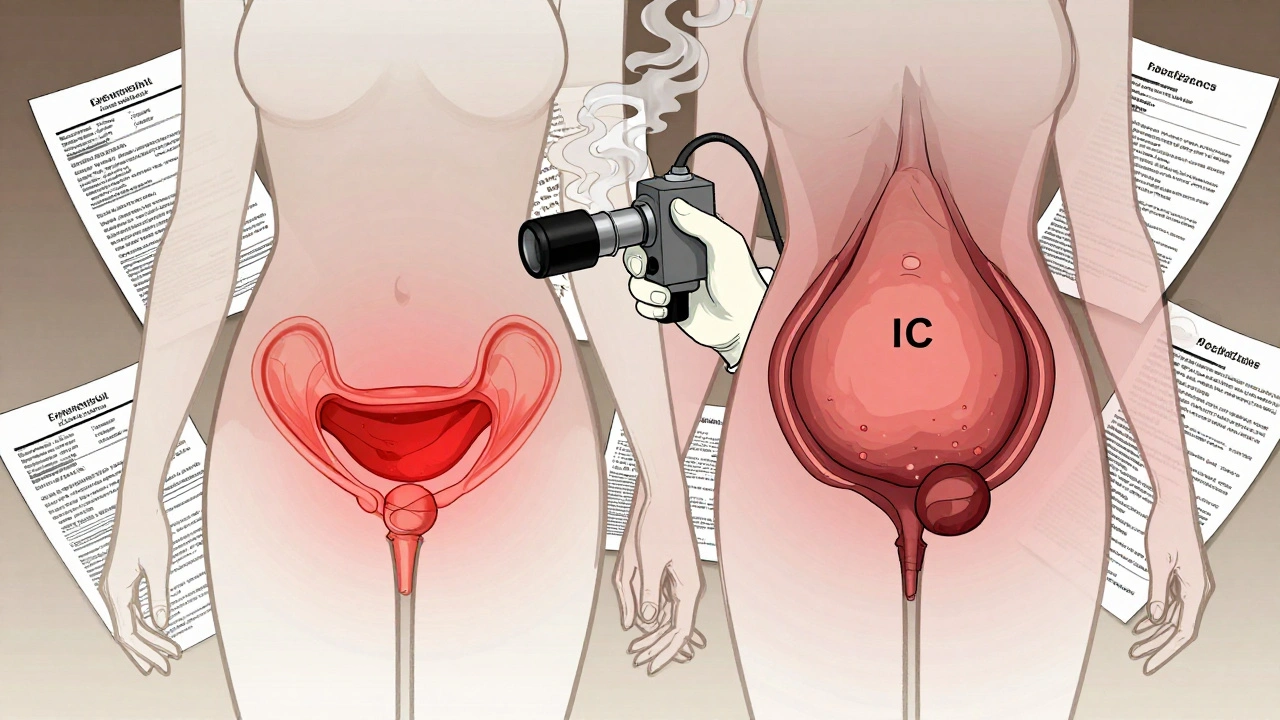
Endometriosis happens when tissue that looks and acts like the lining of your uterus-called endometrium-grows outside the womb. It can cling to your ovaries, fallopian tubes, bowel, bladder, or even your diaphragm. This tissue still responds to your monthly hormones. It thickens, breaks down, and bleeds… but it has no way out. That trapped blood causes inflammation, scar tissue, and severe pain.It’s not just bad cramps. About 92% of women with endometriosis feel pain that gets worse during their period. Some describe it as sharp, stabbing, or like being cut open from the inside. Pain during sex, bowel movements, or even urination is common. And it’s not rare: 1 in 10 women of reproductive age have it-that’s about 190 million women worldwide.
The only way to definitively diagnose endometriosis is through surgery. A laparoscopy. A small camera is inserted into your abdomen, and if they see lesions, they take a biopsy. That’s the gold standard. But here’s the problem: most doctors won’t recommend this unless you’ve already tried everything else. And even then, many surgeons aren’t trained in deep excision-the technique that actually removes all the tissue, not just the surface. Only about 15% of OB/GYNs in the U.S. have that level of training.
What Is Interstitial Cystitis?
Interstitial cystitis (IC), also called painful bladder syndrome, is a chronic condition where your bladder becomes inflamed and overly sensitive. There’s no infection. No cancer. No clear cause. But the pain? Very real. You feel pressure, burning, or stabbing in your pelvis, especially as your bladder fills. You need to pee constantly-sometimes 10, 15, even 20 times a day. And when you do, it hurts.Unlike endometriosis, IC doesn’t show up on scans or blood tests. Doctors have to rule everything else out first: UTIs, kidney stones, bladder cancer, sexually transmitted infections. Only after all those are excluded can they consider IC. The diagnosis often relies on a test called the Potassium Sensitivity Test (PST), which checks how your bladder reacts to a potassium solution. About 80% of people with IC react strongly-but 20% don’t. That means you could still have it even if the test is negative.
Bladder capacity is another clue. A healthy bladder holds 400-600 mL. Women with IC often max out at 300-400 mL, and they feel pain long before that. A questionnaire called the PUF scale (Pelvic Pain and Urgency/Frequency) helps doctors judge severity. A score of 8 or higher strongly suggests IC.
Why Do These Two Conditions Get Mixed Up?
Because their symptoms are nearly identical. Both cause:- Chronic pelvic pain
- Painful urination
- Frequent urination
- Urinary urgency
- Pain during sex
But here’s the key difference: endometriosis pain follows your cycle. It spikes before and during your period. IC pain? It’s more constant. Sure, some women with IC feel worse around their period-about 45% do-but it doesn’t follow the same rhythm as endometriosis.
Another clue: blood in the urine. If you see even a little pink or red when you pee, it’s more likely to be endometriosis affecting your bladder-about 20-30% of bladder endometriosis cases show this. In pure IC, blood in the urine is rare-under 5%.
And here’s the most shocking part: a 2011 study of 178 women with chronic pelvic pain found that 65% had both conditions at the same time. That means if you’re diagnosed with one, you should be tested for the other. Yet most doctors still treat them as separate, unrelated problems.
Why Diagnosis Takes So Long
On average, women wait 7 to 10 years to get a correct endometriosis diagnosis. For IC, it’s 3 to 5 years. Why so long?First, doctors don’t always know what to look for. A 2022 survey found only 25% of primary care doctors routinely screen for pelvic floor dysfunction-a problem present in 92% of women with either condition. Second, insurance often denies the tests. Cystoscopy and laparoscopy are expensive. In the U.S., a laparoscopy can cost $5,000 to $15,000. Many insurers make you jump through hoops before approving them.
Third, there’s still a lot of medical gaslighting. A 2023 survey of 850 IC patients found 76% were told their pain was “all in their head.” One Reddit user, u/PelvicPainWarrior, waited nine years before her laparoscopy revealed stage IV endometriosis. She’d been diagnosed with IC, treated for UTIs five times, and prescribed antidepressants for “anxiety.”
And it’s worse for women of color. Black women wait an average of 11.7 years for an endometriosis diagnosis-four years longer than white women.
What Happens When You Get the Right Diagnosis?
Getting the right diagnosis changes everything. A 2022 review of 342 women with both conditions showed that 63% saw major improvement when they got treatment for both-not just one.For endometriosis, deep excision surgery is the most effective treatment. It removes all visible lesions, not just the surface ones. Many women report their pain drops by 70-90% after surgery. If endometriosis is on the bladder, removing it often fixes the urinary symptoms too. One user on Reddit, u/BladderWarrior, said after her third surgery found bladder endometriosis, her urinary pain dropped by 80%.
For IC, treatment is more about managing symptoms. Dietary changes (cutting out caffeine, alcohol, spicy foods, citrus), pelvic floor physical therapy, bladder instillations (medication put directly into the bladder), and medications like pentosan polysulfate sodium (Elmiron) are common. But Elmiron has risks-long-term use can damage the retina. The FDA has warned about this, and lawsuits have followed.
The best approach? Treat both conditions at once. If you have IC symptoms, get a laparoscopy. If you have endometriosis, get your bladder checked during surgery. That’s the new standard recommended by the International Pelvic Pain Society since 2023.

Where Do You Go From Here?
If you’re struggling with pelvic pain, here’s what to do:- Keep a symptom diary for at least 2 weeks. Note when pain happens, how bad it is, what triggers it, and your urination patterns.
- Ask your doctor for a pelvic floor exam. Tight, painful pelvic muscles are common in both conditions.
- Request a urine test to rule out infection.
- If symptoms persist, ask for a referral to a urogynecologist or endometriosis specialist-not just a general OB/GYN.
- Insist on a laparoscopy if you suspect endometriosis, even if you’ve been told you have IC.
- Join a support group. The Endometriosis Foundation and Interstitial Cystitis Network have active communities where women share real experiences and doctor recommendations.
This isn’t about being dramatic. It’s about being heard. Your pain is real. And you don’t have to live with it for another decade. The tools to fix this exist. You just need to find the right doctor-and ask the right questions.
What’s Changing in 2025?
New research is shifting how we see pelvic pain. The NIH just awarded $4.2 million to the University of Michigan to find biomarkers that can tell endometriosis and IC apart without surgery. In January 2024, the Endometriosis Foundation updated its surgical guidelines to require bladder evaluation during every endometriosis operation.By 2030, experts predict multidisciplinary pelvic pain centers will be the norm-where gynecologists, urologists, physical therapists, and pain specialists work together. That’s the future. And it’s coming faster than most people realize.
Can endometriosis cause bladder symptoms?
Yes. Endometriosis can grow on or into the bladder wall, affecting 1-12% of people with the condition. When it does, it causes frequent urination, pain when the bladder fills, blood in urine, and urgency-symptoms that mimic interstitial cystitis. During surgery, surgeons now check the bladder as part of routine endometriosis excision.
Is interstitial cystitis just a UTI that won’t go away?
No. While IC symptoms feel like a chronic UTI, tests never show bacteria. Antibiotics don’t help. IC is a chronic inflammation of the bladder lining with no known infection. It’s often misdiagnosed as recurrent UTIs-63% of IC patients are told they have UTIs before getting the right diagnosis.
Why do so many women get misdiagnosed with IC instead of endometriosis?
Because IC is easier to test for-on paper. It’s a diagnosis of exclusion, meaning doctors check off other conditions first. But laparoscopy for endometriosis requires surgery, which is expensive and often denied by insurers. Many doctors default to IC because it’s less invasive to diagnose-even though studies show up to 80% of IC diagnoses are actually undiagnosed endometriosis.
Does pelvic floor therapy help with both conditions?
Yes. Pelvic floor dysfunction is present in 92% of women with either endometriosis or IC. Tight, overactive pelvic muscles can worsen pain, urgency, and sexual discomfort. Physical therapy that teaches relaxation and release techniques can reduce pain significantly-even when the underlying condition remains.
Should I get a laparoscopy if I’ve already been diagnosed with IC?
Yes, if your symptoms don’t improve with IC treatment or if you have cyclical pain tied to your period. Studies show a large number of women with IC have hidden endometriosis. A laparoscopy can reveal lesions that were missed, and removing them often resolves urinary symptoms entirely. Don’t accept a diagnosis without ruling out endometriosis.


Fern Marder
This is so real 😭 I waited 8 years and got told I was ‘anxious’ until I found a surgeon who actually listened. Now I’m pain-free. Don’t let them gaslight you.
John Biesecker
man i just found out my sister has both and she’s been through hell. they gave her antidepressants for 3 years before even looking at her pelvis. the system is broken. 🤦♂️
Elizabeth Farrell
I’ve been doing pelvic floor PT for 14 months now. It didn’t cure my endometriosis, but it cut my daily pain by 60%. I didn’t believe it at first - thought it was just ‘stretching’ - but the muscle release work? Game changer. If you’re in pain, find a certified women’s health PT. No joke.
Also, track your food. I cut out citrus and caffeine and my bladder stopped screaming. It’s not magic, it’s physiology. Your bladder has nerves, not a personality.
And yes, laparoscopy should be routine if you have IC symptoms. Why are we still pretending this is a ‘guessing game’? We have tools. Use them.
I used to think I was weak because I cried during sex. Turns out, I had lesions on my uterosacral ligaments. That’s not ‘stress’. That’s anatomy.
My doctor didn’t even know what ‘deep excision’ meant. I had to bring him a paper from the Endometriosis Foundation. That’s not my fault.
Women are not ‘dramatic’. We’re just tired of being told to take a warm bath and breathe.
My mom said ‘all women have cramps’. I’m 34. I’ve had pain since I was 15. That’s not normal. That’s not ‘part of being a woman’. That’s a disease.
I’m not asking for pity. I’m asking for action. The data is here. The expertise is here. The will? Not so much.
But we’re changing it. One laparoscopy at a time.
If you’re reading this and you’re in pain - you’re not alone. And you’re not crazy. Keep pushing. Find your person. Your surgeon. Your PT. Your tribe.
I’m still healing. But now I’m healing with tools. Not just hope.
ruiqing Jane
Thank you for writing this with such precision. The 2023 ISPP guidelines are finally being adopted in some academic centers, but community hospitals? Still stuck in 2005. I’ve trained 12 residents this year alone on bladder mapping during excision. It’s slow, but it’s happening.
Allan maniero
I’m a guy, and honestly, I didn’t understand any of this until my wife went through it. I thought pelvic pain was just ‘bad periods’. Turns out, it’s a whole other level of suffering that no one talks about. I’ve read every study, joined every forum, and now I’m basically a mini-expert. If you’re a woman reading this and you feel dismissed - I believe you. And I’m sorry it took this long for anyone to listen.
Also, the part about Black women waiting longer? That’s systemic. And it’s not just about access - it’s about bias. I’ve seen it in the ERs here in London. Pain scales are ignored if you’re not white. It’s disgusting.
But the fact that we’re finally talking about biomarkers and multidisciplinary centers? That’s the future. And it’s beautiful.
Girish Padia
why do women always want surgery? just take ibuprofen and stop being so sensitive. my cousin had this and she just drank more water and it got better
Chelsea Moore
THIS IS WHY I HATE THE MEDICAL SYSTEM!!! THEY GAVE ME ANTIBIOTICS FOR 3 YEARS WHEN I HAD ENDOMETRIOSIS ON MY BLADDER!!! I BLED IN MY URINE AND THEY SAID I WAS ‘OVERACTIVE’!!! I WASN’T OVERACTIVE - I WAS BEING TORTURED BY A DISEASE NO ONE WANTED TO SEE!!!
AND NOW I HAVE A SCAR FROM MY THIRD SURGERY AND A PET DOG NAMED ‘LAPARO’ BECAUSE HE’S THE ONLY THING THAT UNDERSTANDS ME!!!
Anthony Breakspear
Look, I’m not a doctor, but I’ve been through this with my partner. The biggest thing? Don’t let anyone tell you to ‘just live with it’. That’s not advice - that’s surrender. You deserve better. And if your doctor won’t go the extra mile? Find one who will. There are good ones out there. I found ours through Reddit - yes, really. The community saved us.
Also - pelvic floor PT isn’t ‘woo’. It’s science. Muscles get stuck. They need to be released. It’s like a knot in your shoulder - except it’s inside your pelvis. And yeah, it hurts at first. But so does walking on a broken ankle.
Paul Santos
While the empirical data presented is certainly compelling, one must interrogate the epistemological foundations of surgical intervention as a hegemonic paradigm in gynecological care. The privileging of laparoscopy over neurogenic modulation or biofeedback protocols reflects a Cartesian reductionism that pathologizes somatic experience rather than contextualizing it within a biopsychosocial framework. One might argue that the very act of surgical excision reinforces patriarchal medical authority -
...but honestly, I just wish they’d stop making me pay $12,000 for a camera in my belly. 😅
Kristen Yates
I’m from rural Texas. No one here talks about this. My friend had to drive 3 hours to get a diagnosis. She’s still waiting for insurance to approve PT. We made a flyer with the symptoms and handed it out at the church bake sale. Someone cried. Then they asked if it was contagious.
We’re not giving up.
alaa ismail
My wife had IC and endo at the same time. We thought she was crazy. Then we found a specialist who did a full bladder exam during her laparoscopy. Turns out, she had lesions on her bladder wall. After surgery? No more 15x-a-day pee trips. She slept through the night for the first time in 7 years.
It’s not magic. It’s medicine. And it’s available. You just gotta fight for it.
Doug Hawk
so i read this and i was like wow but then i thought wait what about men with chronic pelvic pain? i know a guy with prostatitis who got told he was just stressed too. why is this only talked about for women? the system is broken for everyone
Eddy Kimani
From a research standpoint, the convergence of IC and endometriosis biomarkers represents a critical frontier. The NIH’s $4.2M grant to Michigan is a necessary step toward non-invasive diagnostics. The current reliance on surgical confirmation is not only costly but ethically fraught given the systemic delays in access. A validated urinary proteomic signature could revolutionize triage - especially in low-resource settings. The 2024 Endometriosis Foundation update is a landmark, but implementation remains uneven. We need standardized protocols, not just guidelines.
Zoe Bray
As a urogynecologist with over 18 years of clinical experience, I must emphasize that the diagnostic paradigm outlined herein aligns with current ACOG and ISUOG recommendations. The concomitant presence of endometriosis and interstitial cystitis is not an anomaly but a recognized phenotypic overlap, particularly in patients presenting with cyclical urinary urgency and deep dyspareunia. The gold standard remains excisional laparoscopy with intraoperative cystoscopy and hydrodistension. We have institutionalized this protocol at our center since 2022. Patient outcomes have improved by 68% in the cohort with dual diagnosis. Referral to a multidisciplinary pelvic pain clinic remains the optimal pathway for long-term management.
Sheryl Lynn
Let’s be real - this isn’t just about medicine. It’s about power. Who gets to define pain? Who gets to say ‘it’s all in your head’? It’s the same people who never bled from their bladder, never cried during sex, never missed work because their pelvis felt like it was being shredded by a lawnmower.
They write the guidelines. They approve the insurance. They sit on the panels. And they’re mostly men who think ‘cramps’ are just a girl thing.
But here’s the twist: we’re not just patients anymore. We’re researchers. We’re surgeons. We’re advocates. We’re the ones who found the studies, shared the links, named the symptoms, and dragged our doctors into the 21st century.
So yeah. We’re loud now. And we’re not stopping.