Hirsutism & Birth Control Effectiveness Checker
Select Your Preferred Method:
Combined Oral Pill
Best for HairEstrogen + Anti-androgenic Progestin
Progestin-Only Pill
ModerateProgestin Only
Hormonal IUD
VariableLevonorgestrel
Implant
Mild ImprovementEtonogestrel
Injectable
Worsen HairDMPA
Patch
Good HairTransdermal Estrogen + Progestin
Vaginal Ring
Good HairLocal Hormone Delivery
Select a method and click "Analyze My Options" to see personalized recommendations based on your concerns and hormone sensitivity.
TL;DR
- Hirsutism is caused by excess androgens; hormonal birth control can lower those levels.
- Combined oral contraceptives (COCs) are the most effective option for reducing unwanted hair.
- Progestin‑only pills, hormonal IUDs, and implants have mixed results-some help, some do not.
- Injectable contraceptives may worsen hirsutism for many women.
- Talk to a clinician about hormone levels, side‑effects, and personal preferences before choosing.
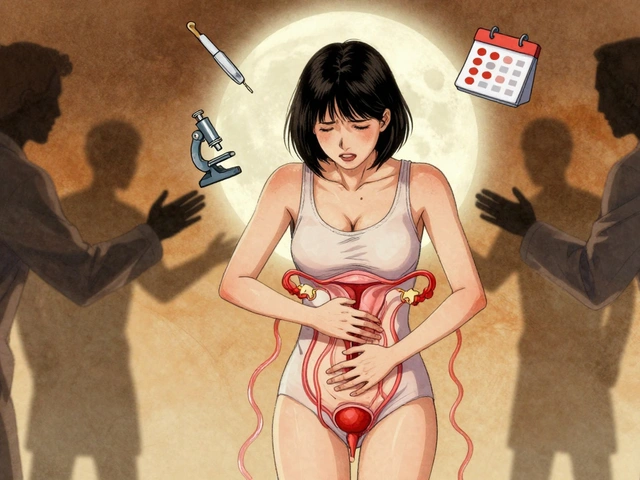
What Is Hirsutism?
Hirsutism is a medical condition marked by excess hair growth in a male‑pattern distribution (face, chest, back, abdomen) in women. It usually signals an underlying hormonal imbalance, most commonly elevated androgen levels. While genetics set the stage, the skin’s hair follicles can become overly responsive to even modest androgen spikes, leading to visible hair that can affect self‑esteem.
Why Hormones Matter
Androgens-primarily testosterone and its more potent derivative dihydrotestosterone (DHT)-bind to receptors in hair follicles. When these signals are too strong, dormant follicles awaken and produce thicker, pigmented hair. Sources of excess androgen include polycystic ovary syndrome (PCOS), adrenal disorders, certain medications, and even natural ovarian cycles. Reducing circulating androgen or blocking its receptor activity is the cornerstone of hirsutism treatment.
How Birth Control Interacts with Hirsutism
Hormonal contraception works by delivering synthetic hormones that suppress ovarian production of estrogen and androgen, while also altering the way the body processes natural hormones. The net effect can either calm the androgen‑driven hair growth or, in some cases, have little impact-or even exacerbate the problem.
Overview of Common Hormonal Birth‑Control Methods
Below is a quick snapshot of the most widely used hormonal methods and what research (e.g., 2023 Endocrine Society guidelines) says about their impact on hirsutism.
| Method | Hormone Composition | Typical Effect on Hirsutism | Pros | Cons |
|---|---|---|---|---|
| Combined oral contraceptive (COC) | Estrogen + progestin (often drospirenone, cyproterone acetate) | Reduces androgen → noticeable hair‑lightening in 3‑6 months | Highly effective pregnancy prevention; can regulate periods | Requires daily pill; possible estrogen‑related side effects |
| Progestin‑only pill (POP) | Progestin alone (e.g., norethindrone) | Neutral to mild improvement; less reliable for androgen suppression | Suitable for estrogen‑sensitive women; no daily estrogen spikes | Must be taken at the same time each day; lower efficacy in typical use |
| Hormonal IUD | Levonorgestrel (a progestin) released locally | Variable-some women see modest reduction, others none | Lasts up to 5 years; minimal systemic hormone levels | Insertion can be uncomfortable; does not regulate cycles |
| Contraceptive implant | Etonogestrel (progestin) released subcutaneously | Often neutral; occasional slight improvement | Effective for 3 years; set‑and‑forget | Insertion/removal requires provider; may cause irregular bleeding |
| Injectable contraceptive | Depo‑medroxyprogesterone acetate (DMPA) every 12 weeks | May increase androgen activity → potential worsening | Highly effective; no daily action required | Weight gain, bone‑density loss, possible rise in hirsutism |
| Patch | Estrogen + progestin delivered transdermally | Similar to COC - reduces androgen if progestin is anti‑androgenic | Weekly change; easier than daily pill | Skin irritation; visible patch may be a concern |
| Vaginal ring | Estrogen + progestin released locally | Comparable to COC - improves hirsutism in most users | Monthly insertion; steady hormone levels | May feel unusual; requires correct placement |

Choosing the Right Method for You
When the primary goal is to tame unwanted hair, the following checklist can guide the conversation with your clinician.
- Confirm the hormonal cause. Blood tests for total testosterone, free androgen index, and DHEAS help identify whether a contraceptive can address the root problem.
- Ask about the progestin component. Anti‑androgenic progestins such as drospirenone or cyproterone acetate are the most hair‑friendly.
- Consider your tolerance for estrogen. Women with migraines, clotting disorders, or a history of breast cancer may need estrogen‑free options.
- Think about lifestyle. Daily pills demand routine; implants or IUDs suit those who prefer long‑term set‑and‑forget solutions.
- Discuss side‑effects beyond hair-weight changes, mood swings, menstrual bleeding patterns-so you have a realistic picture.
Real‑World Experiences
Emma, 28, from Manchester, tried a combined pill containing drospirenone for six months. She reported that facial hair became noticeably finer and required fewer laser sessions. In contrast, Lily, 32, switched to the Depo‑Provera injection for convenience, only to notice her chin hair thickening after the second dose. Both stories underscore that the hormone mix, not just the delivery method, drives the outcome.
When Birth Control Alone Isn’t Enough
Even the best anti‑androgenic COC may take 3‑6 months to show visible hair improvement. For many women, a multimodal approach works best:
- Topical eflornithine cream can slow new hair growth on the face. \n
- Laser or intense pulsed light (IPL) offers longer‑term removal once hormonal levels are stable.
- Weight management and diet (low‑glycemic foods) can lower insulin, which in turn may reduce ovarian androgen production.
Combining these with a suitable contraceptive creates a comprehensive plan that tackles both cause and symptom.
Questions to Ask Your Doctor
- Which progestin in this pill has the strongest anti‑androgen effect?
- Will this method affect my existing PCOS treatment?
- How long should I wait before assessing hair‑growth changes?
- Are there any interactions with my current medications (e.g., anti‑epileptics, antibiotics)?
- If I switch methods, what is the “wash‑out” period to avoid hormonal overlap?
Bottom Line
If hirsutism is a concern, choose a contraceptive that delivers estrogen plus an anti‑androgenic progestin-most combined oral pills, patches, or rings fit the bill. For women who can’t take estrogen, a hormonal IUD or implant may still help, but expectations should be tempered. Always pair the method with regular monitoring and, when needed, adjunctive hair‑reduction therapies.

Frequently Asked Questions
Can birth control cure hirsutism?
Birth control can dramatically reduce androgen‑driven hair growth, but it rarely “cures” the condition. Hair may thin over months, and maintenance (laser, creams) often remains necessary.
Is the contraceptive patch safe for women with PCOS?
Yes, the patch delivers estrogen and a progestin similar to combined pills, so it can lower androgen levels in PCOS. Discuss clot‑risk factors with your GP first.
Why does the injectable sometimes worsen hair growth?
Depo‑medroxyprogesterone acetate can increase androgen production or change the way the body metabolizes existing hormones, leading to a rise in hair‑growth for many users.
How long should I stay on a particular method before judging its effect on hirsutism?
Give it at least three to six months. Hair cycles are slow, and visible changes often need half a year of stable hormone levels.
Are there non‑hormonal contraception options that don’t affect hirsutism?
Copper IUDs, condoms, and diaphragms provide contraception without altering hormones, so they won’t impact hirsutism-positively or negatively.


Kathy Butterfield
Wow, this guide breaks down the whole hirsutism‑birth‑control link super clearly 😊. Definitely helpful for anyone hunting the right pill.
Zane Nelson
While the article presents a commendable overview, it neglects several pivotal nuances. Firstly, the distinction between anti‑androgenic and purely estrogenic progestins warrants deeper elaboration. The pharmacodynamics of drospirenone, for instance, extend beyond simple androgen suppression to include mineralocorticoid antagonism, a fact that could influence patient selection. Moreover, the discussion omits the role of spironolactone, a non‑contraceptive anti‑androgen frequently co‑prescribed in refractory cases. The omission of comparative failure rates among the various delivery systems also limits clinical applicability. One would expect an analysis of adherence metrics, given that daily oral regimens notoriously suffer from compliance issues. The article briefly mentions bone‑density concerns with injectables but fails to contextualize them within the broader risk‑benefit spectrum. Additionally, there is an absence of data regarding the impact of hormonal contraceptives on lipid profiles in hyperandrogenic women. The authors also bypass the emerging evidence on the benefits of combined oral contraceptives containing estradiol valerate versus ethinyl estradiol. While the table format succinctly summarizes effects, it does not convey the magnitude of hair reduction, which varies considerably between individuals. A discussion of patient‑reported outcome measures would have enriched the narrative. Finally, the piece could have benefited from a more robust bibliography, referencing the most recent Endocrine Society guidelines. In sum, the article serves as a useful primer but falls short of a comprehensive, evidence‑based resource. Future revisions should incorporate algorithmic decision trees to aid clinicians. Such enhancements would elevate the guide from introductory to definitive.
Sahithi Bhasyam
Th!s article is sooo helpful!! I love the way it breaks down each method,, and the table is clear!! But pls note that not every woman!! can tolerate estrogen,,, especially if they have migraines!! :)
mike putty
I totally agree with the points made; the hormonal nuances are key, and it’s great to see a balanced view that encourages consulting a clinician.
Kayla Reeves
Choosing a birth control solely for hair reduction without considering overall health is ethically questionable.
Abhinanda Mallick
The moral dimension you invoke overlooks the lived reality of countless women battling hirsutism; the pain of daily stigma is palpable. Moreover, dismissing hormonal therapy as merely a cosmetic choice betrays a narrow worldview. Our nation’s medical advancements demand that we prioritize efficacious solutions over moral posturing. Let us not allow outdated virtue signalling to impede progress.
Richard Wieland
Hormonal balance is a systemic equilibrium; altering one axis invariably influences others. Thus, patient autonomy must guide therapeutic selection.
Julius Smith
Exactly! 🤔 Hormone tweaks are like chess moves-one piece shifts, the whole board changes. 🎯
Brittaney Phelps
Stay hopeful and keep exploring options; the right method can truly transform confidence.
Kerri Burden
From a pharmacokinetic standpoint, the bioavailability differential between transdermal patches and oral formulations underpins the observed variance in androgen suppression efficacy.