When you pick up a pill bottle from the pharmacy, do you ever wonder why a $4 generic tablet feels less effective than a $12 brand-name version-even though both contain the exact same active ingredient? This isn’t just in your head. It’s the placebo effect at work, and it’s reshaping how millions of people experience their medications every day.
Let’s be clear: generic drugs are not inferior. The FDA requires them to deliver the same amount of active ingredient into the bloodstream as the brand-name version, within a tight 80-125% range. In lab tests, they’re identical. But when real people take them, something strange happens. A 2014 study from the University of Auckland tracked 87 college students with recurring headaches. One group got placebo pills labeled as a brand-name painkiller. Another got the exact same pills labeled as a generic. The brand-labeled placebos reduced pain by 2.3 points on a 10-point scale-almost as much as real ibuprofen. The generic-labeled ones? Just 1.1 points. The pills were identical. The only difference was the label.
Price Tells Your Brain What to Expect
Your brain doesn’t just react to chemicals. It reacts to context. Price is one of the strongest signals it uses. In a 2014 study at the University of Cincinnati, Parkinson’s patients were given fake injections labeled as either a $1,500 treatment or a $100 one. Both were saline solutions. The $1,500 group showed 28% more improvement in movement. Brain scans confirmed their dopamine levels spiked higher-because their brains believed they were getting something better. The same pattern shows up with painkillers. In a Harvard experiment, people told they were getting a $2.50 painkiller reported 37% less pain than those told it cost $0.10-even though both were sugar pills.
This isn’t about greed or marketing. It’s about evolution. For thousands of years, expensive things were better. A finely crafted tool lasted longer. A rare herb healed faster. Your brain still uses price as a shortcut to judge quality. When you see a generic labeled “$0.25 per pill,” your subconscious doesn’t see cost savings. It sees low value.
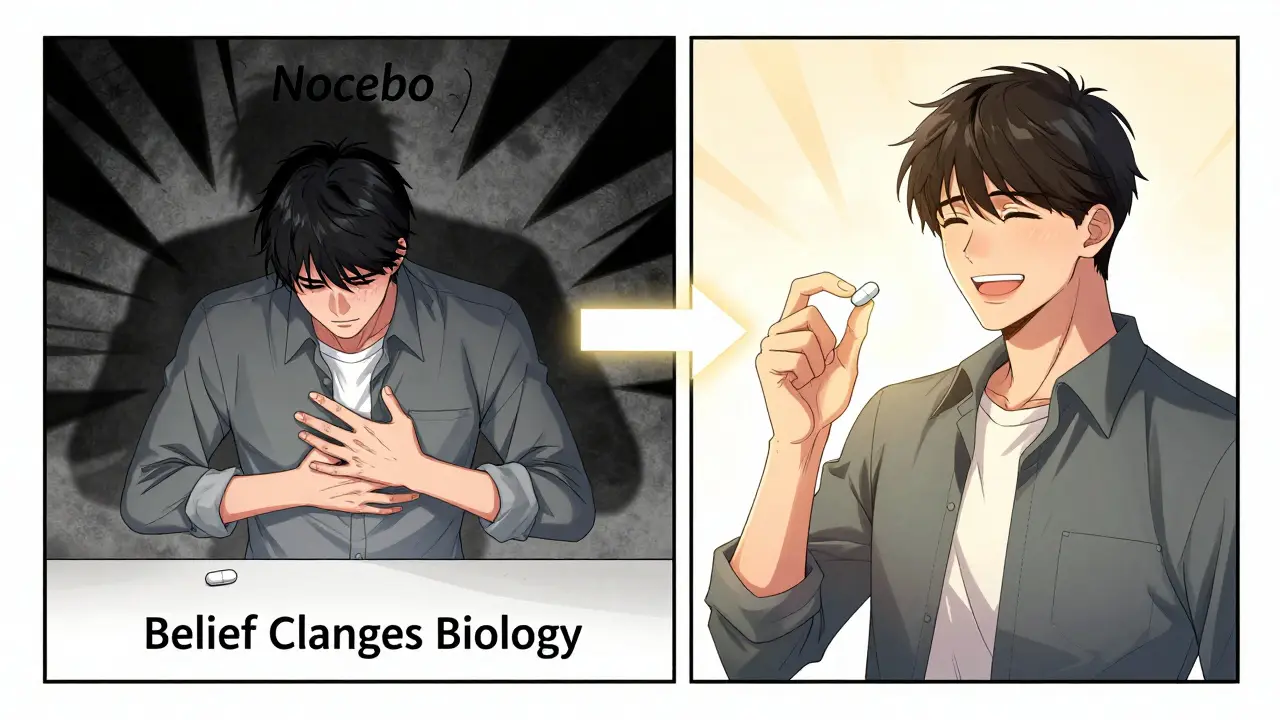
The Nocebo Effect: When Your Mind Makes You Sick
Just as belief can make you feel better, belief can make you feel worse. This is the nocebo effect-the dark twin of the placebo effect. A 2014 meta-analysis of 12 statin trials found that when patients were told they were taking a generic version, they reported 2.1 times more muscle pain than those told they were taking the brand. The pills were identical. The only thing that changed was the label. In another study, 13.2% of people on generic-labeled placebos complained of muscle pain. Only 6.3% did on brand-labeled placebos. That’s not side effects. That’s expectation.
It gets worse in mental health. A 2013 review in Lancet Psychiatry found antidepressant trials with generic labeling had 11% lower response rates than those with brand labels. Patients didn’t just feel less improvement-they felt worse. One Reddit user wrote: “Switched from brand Nexium to generic and my GERD symptoms came back. My doctor said it’s probably nocebo.” He wasn’t lying. His brain just didn’t trust the pill.
Generics Work-If You Believe They Do
Here’s the flip side: when people are told the truth, they do just fine. A 2022 Drugs.com survey of over 8,000 people found that 67% said generics worked just as well as brand-name drugs. But when those same people were given a simple 30-second explanation about bioequivalence-“This generic has the same active ingredient, same dose, same effect”-the number jumped to 82%. Knowledge changes perception.
Doctors who use “positive generic messaging” get better results. In a 2020 trial, physicians trained to say things like, “This generic works exactly the same but saves you money,” saw 85% of patients stick with their medication. Those who just said, “We’re switching you to a generic,” got only 63% adherence. The difference wasn’t in the drug. It was in the words.

Why Some Conditions Are More Sensitive
Not all drugs are affected equally. Placebo effects are strongest in conditions where symptoms are subjective: headaches, depression, anxiety, chronic pain, and epilepsy. In migraine studies, brand-labeled placebos reduced pain by 41%. Generic-labeled ones? Just 22%. But for infections like strep throat or pneumonia? The placebo effect barely matters. If the antibiotic kills the bacteria, you’ll feel better regardless of the label.
This is why the problem hits hardest in mental health and neurological care. These conditions rely heavily on brain chemistry-and your brain’s expectations directly influence that chemistry. Dopamine, serotonin, endorphins-they all respond to belief. If you think the pill won’t work, your brain won’t release the chemicals needed to make you feel better.
Real Consequences, Real Costs
This isn’t just about feeling better. It’s about survival. A 2017 analysis of 38,000 Medicare patients found that people on generic medications had 12-15% higher hospitalization rates than those on brand-name drugs. Not because generics were less effective. Because people stopped taking them. They thought they weren’t working. They felt side effects that weren’t there. They switched back to expensive brands-or quit altogether.
The financial toll is staggering. The U.S. spends $1.2 billion extra each year on unnecessary brand-name prescriptions because people distrust generics. And when people stop taking their meds due to nocebo effects, the healthcare system loses another $318 billion annually in avoidable ER visits, hospital stays, and complications.
What’s Being Done About It?
Some solutions are simple. A 2023 study in Wisconsin tested generic pills in packaging that looked like brand-name bottles-same colors, same font, same logo style. Nocebo complaints dropped by 37%. People didn’t need a lecture. They just needed the pill to look like it belonged.
Another innovation? The FDA’s “Generic Confidence” app. It uses augmented reality to show patients a 3D model of their generic drug, then overlays the brand-name version to prove they’re identical. In beta testing, users were 29% more likely to stick with their prescription.
But the biggest fix? Education. A 2018 study showed that just seven minutes of clear, calm explanation from a doctor raised generic acceptance from 58% to 89%. Patients didn’t need jargon. They needed to know: “This is not a cheaper version. It’s the same drug. The same science. The same results.”
What You Can Do
- If you’re switching to a generic, ask your doctor to explain why it’s the same. Don’t just accept the change-understand it.
- If you feel worse after switching, don’t assume it’s the drug. Talk to your provider. It might be your brain, not the pill.
- If you’re on a long-term medication like blood pressure or antidepressants, track your symptoms before and after the switch. Often, there’s no real difference.
- Use apps like GoodRx or Drugs.com to compare prices and read real patient reviews-not just fear-based stories.
The truth is simple: your mind is powerful. It can turn a sugar pill into a miracle cure. It can turn a lifesaving drug into a source of pain. The difference between a generic and a brand isn’t in the chemistry. It’s in the story you tell yourself.
Are generic drugs really as effective as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. The FDA requires them to deliver the same amount of medicine into your bloodstream within a narrow range (80-125%) of the brand. In over 98% of cases, they work identically. The only differences are in inactive ingredients (like fillers or dyes), which rarely affect how the drug works.
Why do some people feel worse on generic medications?
It’s often the nocebo effect. If you believe generics are inferior, your brain can trigger real physical symptoms-like headaches, nausea, or fatigue-even when the drug is chemically identical. A 2014 study found people on generic-labeled placebos reported twice as much muscle pain as those on brand-labeled ones, despite both being inert. Your expectations shape your experience. Talking to your doctor about this can help break the cycle.
Can the packaging of generic drugs affect how well they work?
Yes. A 2023 trial showed that when generic pills were packaged to look like brand-name versions-same colors, fonts, and design-patients reported 37% fewer side effects and were more likely to keep taking them. Your brain uses visual cues to judge quality. A plain white pill in a basic bottle feels less trustworthy than one that looks polished and familiar. Packaging doesn’t change the chemistry, but it changes your belief-and that changes your body’s response.
Do insurance companies force people to take generics?
In 42% of U.S. states, insurers can require you to switch to a generic without your consent-unless your doctor writes a “dispense as written” note. This is legal under pharmacy benefit rules. But if you’re worried about side effects or feel worse after switching, you have the right to ask your doctor to challenge the substitution. Many doctors will do so if you explain your concerns clearly.
Is there a way to train myself to trust generics?
Yes. Start by learning the science. Read the FDA’s fact sheet on generics. Talk to your pharmacist. Use apps like Drugs.com to see what other patients report. Keep a simple journal: note how you feel before and after switching. You’ll likely find no difference. Over time, your brain will update its belief. Knowledge replaces fear. And when your brain trusts the pill, your body responds accordingly.




Write a comment