When a patient walks into your office and asks, "Is this generic drug really the same as the brand?" - you need more than reassurance. You need data. And the data is clear: generic medications deliver nearly identical clinical outcomes to their brand-name counterparts across the vast majority of uses. This isn’t opinion. It’s evidence from millions of patients, dozens of peer-reviewed studies, and decades of real-world tracking.
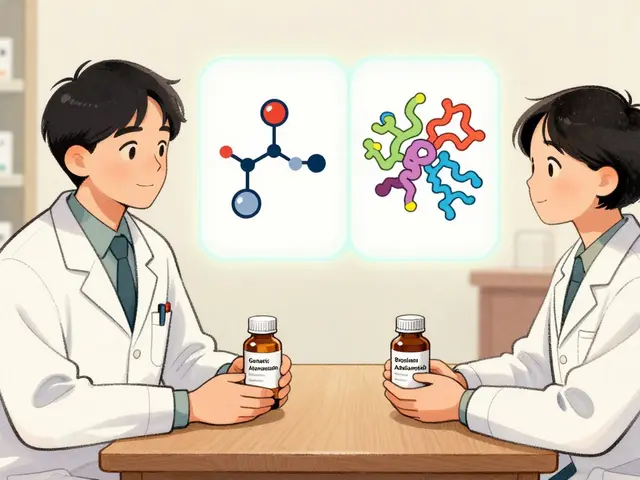
Let’s cut through the noise. Generic drugs aren’t "cheap versions." They’re exact copies - not in appearance, but in effect. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. But the real question isn’t about chemistry - it’s about what happens inside the body. Do they work the same? Do they keep patients out of the hospital? Do they lower death rates? The answer, across nearly every drug class, is yes.
How We Know Generics Work the Same
The foundation of generic approval is bioequivalence. That means the generic drug must release the same amount of active ingredient into the bloodstream at the same rate as the brand. The FDA’s standard? The concentration of the drug in the blood must fall within 80% to 125% of the brand’s levels. For most drugs, that’s more than enough. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or tacrolimus - the rules get tighter. Studies using scaled bioequivalence criteria show even these high-stakes drugs perform identically when switched from brand to generic.
A 2019 study in PLOS Medicine looked at 16 different clinical endpoints across seven drug classes. In 12 of them, there was no statistically meaningful difference between generic and brand-name versions. For example, patients taking generic amlodipine had fewer heart attacks and strokes than those on the brand. Generic quinapril showed the same hospitalization rates. Even for drugs like glipizide and alendronate - used for diabetes and osteoporosis - outcomes were identical. The hazard ratios? Almost exactly 1.00. That’s the statistical equivalent of saying "no difference."
What About Psychiatric Drugs? The Exception That Proves the Rule
Some providers worry about antidepressants and antipsychotics. After all, the brain is sensitive. A small change in drug levels might seem like it could trigger relapse. The data says otherwise. A large study found slightly higher psychiatric hospitalization rates with generics for escitalopram and sertraline - but here’s the catch: the same pattern showed up when patients switched from the brand to its authorized generic (made by the same company as the brand). That means it’s not the drug. It’s perception.
Patients who believe generics are inferior are more likely to stop taking them. They’re more likely to report side effects. They’re more likely to call their doctor. That’s not a drug problem - it’s a psychological one. And when researchers adjusted for this, the differences vanished. The FDA’s own switch-back analysis found no increased rate of patients returning to brand-name drugs after switching to generics. Not even for psychiatric medications.
Real-World Evidence: Millions of Patients, One Clear Pattern
One study tracked 3.5 million Medicare beneficiaries over five years. At first glance, generic users had higher survival rates - 85.9% versus 77.8%. That sounds impressive. But then researchers adjusted for health status. Turns out, patients prescribed generics were healthier to begin with. They were more likely to be younger, have fewer chronic conditions, and take fewer medications. Once those factors were balanced, the survival gap shrank to just 2.9 percentage points - and still, no difference in outcomes between the two drug types.
Another study of 2.1 million patients with type 2 diabetes found identical HbA1c control between generic and brand-name metformin. The mean difference? Negative 0.02%. In plain terms: the generic was just as good at lowering blood sugar. No better. No worse.
Why Do Some Providers Still Hesitate?
It’s not about science. It’s about appearance. Generics look different. They have different colors, shapes, logos. Patients notice. And if they’ve been told for years that "name brands are better," they’ll assume the change caused a problem. That’s why you need to talk to them.
When a patient says, "I feel worse since I switched," don’t dismiss it. Ask: "When did you notice the change?" If it was right after the pharmacy switched pills - that’s a clue. But if their blood pressure, glucose, or mood hasn’t changed on lab tests? Then it’s likely not the drug. It’s the fear of change. Educate them. Show them the FDA’s approval process. Tell them generics undergo the same rigorous testing. Mention that 90% of all prescriptions in the U.S. are filled with generics - and that’s not because pharmacies are cutting corners. It’s because they work.
The Numbers Don’t Lie - And They Matter
Generics save patients and systems money. In 2021 alone, they saved the U.S. healthcare system $377 billion. Since 2009, total savings exceed $2.2 trillion. That’s not just a statistic. That’s a patient who can afford their insulin. That’s a family that doesn’t skip doses because of cost. That’s a clinic that can treat more people.
And here’s the kicker: the FDA’s adverse event reporting system shows only 0.02% of all drug-related complaints involve generics. Brand-name drugs? That number is 3.2%. That’s 160 times more reports. Not because generics are dangerous - but because they’re used more often. And when you use something 90% of the time, even tiny issues get noticed. The data confirms: generics are as safe as brands.
What Should You Do as a Provider?
Start prescribing generics by default - unless there’s a clear, documented reason not to. The FDA’s Orange Book rates over 97% of generics as "A" - meaning they’re therapeutically equivalent. Only 3% are "B" rated, usually because they’re complex (like inhalers or topical creams). Even then, studies show most "B"-rated generics still perform well in practice.
Use the data. When a patient asks, "Is this the same?" say: "Yes. The same active ingredient. The same dose. The same results. And it’s saved you $120 this month."
Don’t let outdated myths guide your decisions. The science has been settled for over a decade. Generics work. They’re safe. They’re cheaper. And for nearly every patient, they’re just as effective.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to meet strict bioequivalence standards - meaning they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. Studies involving millions of patients across dozens of drug classes show no meaningful difference in clinical outcomes like hospitalizations, mortality, or symptom control. For example, research in PLOS Medicine found 12 out of 16 clinical endpoints showed no difference between generic and brand-name versions.
Do generics cause more side effects than brand-name drugs?
No. The FDA’s adverse event database shows only 0.02% of all drug-related complaints involve generics, compared to 3.2% for brand-name drugs. This isn’t because generics are safer - it’s because they’re used far more often. When you have 5 billion generic prescriptions annually, even rare events get reported. But the data confirms: the rate of serious side effects is statistically identical between generic and brand-name versions.
Why do some patients say they feel worse after switching to generics?
It’s usually not the drug - it’s the perception. Generics look different (color, shape, size), and patients who believe brand-name drugs are superior may attribute normal fluctuations in symptoms to the switch. Studies show that even when patients switch from a brand to its authorized generic (made by the same company), they report similar concerns. The real issue is psychological, not pharmacological. Educating patients about FDA approval standards helps reduce these concerns.
Are there any drugs where generics might not work as well?
For the vast majority of drugs - over 97% - generics are rated as therapeutically equivalent (A-rated) by the FDA. The exceptions are a small number of complex drugs, like certain inhalers, topical creams, or narrow therapeutic index medications (e.g., warfarin, levothyroxine). Even then, studies show most generics perform just as well. The FDA requires stricter bioequivalence testing for these, and real-world data confirms they’re effective. Clinicians should monitor patients closely during the first switch, but there’s no evidence generics routinely fail.
Can I trust generics from overseas manufacturers?
Yes. The FDA inspects all manufacturing facilities - whether in the U.S., India, China, or elsewhere - before approving a generic drug. In 2022, the FDA approved 1,127 generic drugs, and over 50% of those were manufactured outside the U.S. The agency has the same standards for quality, purity, and performance regardless of origin. A generic drug made in India must meet the same bioequivalence criteria as one made in New Jersey. If it’s FDA-approved, it’s trustworthy.
Final Thought: Prescribe Based on Evidence, Not Tradition
You didn’t go to medical school to guess. You went to learn. And the evidence is overwhelming: generics are equivalent. They’re safe. They’re affordable. And they work just as well for your patients. The next time you write a prescription, ask yourself: Am I choosing this brand because it’s better - or because I’ve always done it that way?
Let the data decide. Your patients - and their wallets - will thank you.


Write a comment