When a patient skips a dose because the pill costs too much, it’s not just a personal choice-it’s a system failure. Medication nonadherence isn’t rare. In fact, one in three Americans admit to skipping, cutting, or delaying prescriptions because of cost. And the fix isn’t complicated: lower generic drug prices lead directly to better adherence, fewer hospital visits, and billions saved across the healthcare system.
Why Patients Skip Their Medication
People don’t stop taking their meds because they forget. They stop because they can’t afford them. A 2023 JAMA Network Open survey of over 2,100 adults found that 32.7% had skipped doses, delayed refills, or used someone else’s pills to save money. That’s not negligence-it’s rational behavior under financial pressure. The problem starts with how insurance works. Most plans use tiered formularies. A generic statin might cost $5 at the pharmacy. The brand-name version? $75. That’s not a price difference-it’s a barrier. Patients with diabetes, high blood pressure, or arthritis often face dozens of monthly prescriptions. When each one adds up, the math becomes impossible. One Reddit user, u/HeartHealthJourney, shared: “After switching from brand-name Crestor ($75 copay) to generic rosuvastatin ($5 copay), I went from missing 3-4 doses a week to perfect adherence for 11 months straight.”Generic Drugs Aren’t Cheap Copies-They’re the Same Medicine
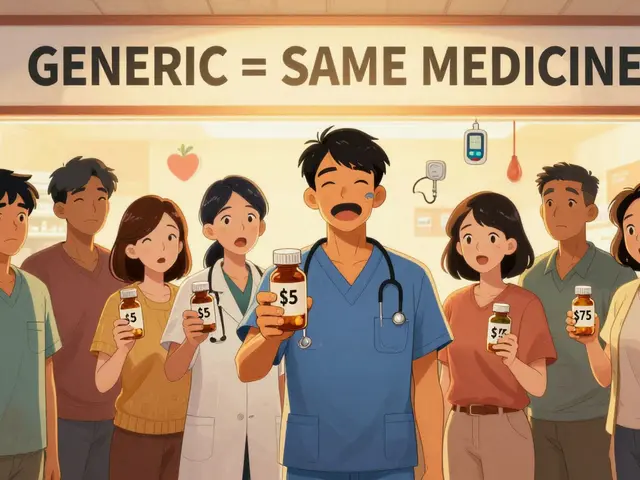
Many patients worry that generics are weaker or less effective. That’s a myth. The FDA requires generic drugs to have the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80% to 125% of the brand. That’s not “close enough.” That’s bioequivalence. The cost difference? Generics cost 80% to 85% less. For example, the brand-name cholesterol drug atorvastatin (Lipitor) used to cost over $200 a month. The generic? Under $10. The result? A 2012 study by Dr. J. Chen tracked Medicare Part D patients after their statins moved from a higher-cost tier to the lowest tier. Adherence jumped by 5.9%. That’s not a small change. It’s life-saving.Every $10 Increase in Cost = Less Adherence
It’s not just about brand vs. generic. It’s about how much the patient pays out of pocket. Research published in the Journal of Managed Care & Specialty Pharmacy found a clear pattern: for every $10 increase in copay, adherence drops by 2% to 4%. That’s a direct, measurable line from price to behavior. For GLP-1 receptor agonists used to treat type 2 diabetes, a 2023 study in Diabetes Care found that each $10 rise in out-of-pocket cost reduced adherence by 3.7%. And what happens when people stop taking these drugs? Emergency room visits go up by 5.2%. That’s not just bad for the patient-it’s bad for the system. Nonadherence contributes to up to 50% of treatment failures and leads to more than 100,000 preventable deaths every year in the U.S.How Lower Costs Save Money-Even When Drug Spending Goes Up
It sounds counterintuitive, but when patients take their meds as prescribed, total healthcare spending drops. Why? Because they end up in the hospital less. A 2011 study by Roebuck et al. in Health Affairs showed that adherent patients had 15% to 20% fewer hospitalizations. For chronic conditions like heart disease, diabetes, and depression, consistent medication use prevents complications that cost thousands-sometimes tens of thousands-per episode. The numbers tell the full story: generic drugs make up 90% of prescriptions filled in the U.S., but only 23% of total drug spending. From 2009 to 2019, they saved the system $643 billion. That’s not a rounding error. That’s enough to cover the entire Medicare Part D program for over a year.
Real-World Impact: Breast Cancer, Heart Disease, and Mental Health
The data isn’t abstract. It’s lived. In a 2011 study on aromatase inhibitors for early-stage breast cancer, patients on brand-name drugs had a 22.3% discontinuation rate. Those on generics? 17.8%. Adherence rates were 68.4% vs. 73.1%. That difference? It’s the difference between survival and recurrence. The same pattern holds for blood pressure and antidepressants. A 2022 systematic review of 160 studies found that higher cost-sharing consistently led to lower adherence-especially for cardiovascular, mental health, and diabetes medications. These are conditions where missing a dose doesn’t just mean feeling off-it means stroke, heart attack, or suicide risk goes up.What’s Working: Policy Changes and Tools That Help
Change is happening. The Inflation Reduction Act of 2022 capped insulin at $35 a month. Starting in 2025, Medicare Part D will have a $2,000 annual out-of-pocket cap. That’s going to help 1.4 million seniors stay on their meds. Real-time benefit tools (RTBTs) are another game-changer. These tools show doctors the exact cost of a prescription before they write it. In pilot programs, they’ve improved adherence by 12% to 15%. One pharmacy program, Magellan’s inforMED, reported a 40% reduction in care gaps and a 2:1 return on investment. But tools alone aren’t enough. Patients need to understand that generics aren’t second-rate. The FDA’s “It’s Okay to Use Generics” campaign helps. So do apps like GoodRx, which show price differences between pharmacies in real time.Why This Matters More Than Ever
Americans pay 256% more for brand-name drugs than people in other developed countries. Between 2022 and 2023, nearly half of all drug prices rose faster than inflation. The average increase? $590 per product. Meanwhile, therapeutic duplication-prescribing two drugs for the same condition-is still costing the system 20% to 30% more than needed. Better coordination between doctors, pharmacists, and patients could fix that too. The solution isn’t about more drugs. It’s about better access. When a patient can afford their medicine, they take it. When they take it, they stay healthy. When they stay healthy, the system saves money. It’s not magic. It’s math.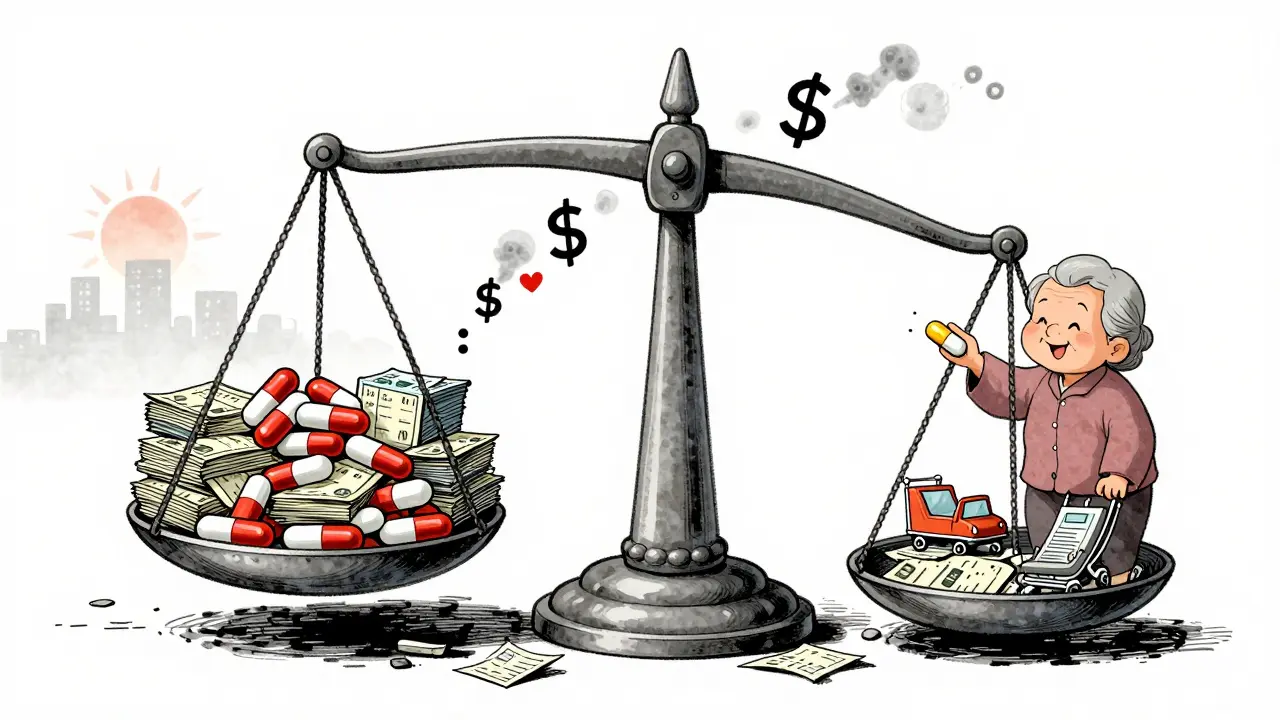
What Patients Can Do Today
If you’re struggling to afford your meds:- Ask your doctor if a generic version is available.
- Use GoodRx or SingleCare to compare prices at nearby pharmacies.
- Ask about patient assistance programs-many drugmakers offer free or discounted meds to those who qualify.
- Don’t be afraid to ask: “Is there a cheaper alternative that works just as well?”
- If your insurance denies coverage, appeal. Many denials are overturned.
What Providers Can Do
Doctors and pharmacists aren’t just prescribers-they’re advocates. Use real-time benefit tools. Ask patients about cost before writing a script. If a patient says they can’t afford a med, don’t just nod. Offer alternatives. Connect them to resources. That’s care.It’s Not About Saving Money-It’s About Saving Lives
Lower generic prices aren’t a policy debate. They’re a public health imperative. Every time a patient fills a prescription because it’s affordable, they’re less likely to end up in the ER. Less likely to be hospitalized. Less likely to die prematurely. The data is clear. The solutions exist. What’s missing is the will to act.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80% to 125% of the brand-name drug’s performance. Generics are not cheaper because they’re weaker. They’re cheaper because they don’t require the same marketing, research, and patent costs.
Why do some patients still prefer brand-name drugs even when generics are cheaper?
Some patients believe brand-name drugs work better due to marketing or personal experience-even though there’s no clinical difference. Others worry about inactive ingredients or packaging changes. A few may have had a bad reaction to a generic in the past, though that’s rare. Education and trust-building with providers help reduce these concerns. The FDA’s "It’s Okay to Use Generics" campaign is one step toward correcting misinformation.
How much can I save by switching to a generic medication?
On average, you can save 80% to 85%. For example, a brand-name statin might cost $200 a month, while the generic costs under $10. Even with insurance, copays for brand-name drugs often range from $50 to $100, while generics are typically $5 to $20. Over a year, that’s $1,000 to $2,000 in savings.
Do insurance plans always cover generic drugs at the lowest cost tier?
Not always. Some plans still place certain generics in higher tiers, especially if they’re newer or if the manufacturer has deals with insurers. Always check your plan’s formulary. If a generic isn’t in the lowest tier, ask your doctor to request a tier exception. Many insurers will approve it if you show the cost difference is a barrier to adherence.
Can switching to a generic medication cause side effects?
Rarely. The active ingredient is identical. But inactive ingredients (like fillers or dyes) can differ. In very rare cases, someone may react to one of those. If you notice a new side effect after switching, tell your doctor. But don’t assume the generic is the problem-sometimes it’s just a coincidence. Your doctor can help determine if it’s a true reaction or something else.
What should I do if I can’t afford my medication even with a generic?
Ask your pharmacist or doctor about patient assistance programs. Many drugmakers offer free or low-cost meds to people with low income. You can also check NeedyMeds.org or the Partnership for Prescription Assistance. Some pharmacies offer discount programs for common generics-for example, Walmart and Target sell many generics for $4 to $10 a month. Don’t skip doses. Talk to someone who can help.



Donna Fleetwood
Just had my first generic statin refill last week-$4 at Walmart. I used to skip doses because the brand was $80. Now I take it like clockwork. My BP’s down, my anxiety’s down, and I’m actually sleeping through the night. It’s not magic, it’s just… affordable.
Shubham Dixit
Let me tell you something about America’s healthcare mess. You think generics are the answer? Try looking at how India produces 40% of the world’s generics-without the corporate greed. Here, Big Pharma owns the FDA, the insurers, and even your doctor’s prescription pad. We need to stop treating medicine like a luxury good and start treating it like a human right. If you’re paying $200 for a pill that costs $2 to make, you’re being robbed. And no, ‘market forces’ won’t fix this. Only systemic change will.
KATHRYN JOHNSON
Incorrect. The FDA’s bioequivalence standard is 80–125%, but that’s a confidence interval-not a guarantee of identical effect. Some patients report clinically significant differences, especially with narrow-therapeutic-index drugs like levothyroxine or warfarin. The data you cite ignores individual pharmacokinetic variation. This isn’t about cost-it’s about clinical nuance. Don’t oversimplify.
Blair Kelly
My uncle died because he switched to a generic antidepressant and started having hallucinations. He told his doctor. They told him it was ‘in his head.’ He stopped taking it. Then he jumped off a bridge. Generic drugs aren’t ‘the same.’ They’re a gamble. And someone’s kid, parent, or spouse is paying for that gamble every single day. This isn’t a spreadsheet-it’s blood on the floor.
Rohit Kumar
In my country, we don’t have this problem because medicine is treated as a public good, not a profit center. A man in rural Bihar pays less than $0.10 for a month’s supply of metformin. He doesn’t need GoodRx-he needs dignity. The real tragedy isn’t the price of pills-it’s that we’ve convinced ourselves that human life has a market value. When your system requires you to choose between food and insulin, you’re not a patient-you’re a statistic being optimized.
Sheila Garfield
My mum’s on blood pressure meds. She used to skip them ‘till payday.’ Now she takes them every day because her local pharmacy runs a $4 generic program. She says it’s the first time in 15 years she’s felt ‘normal.’ No drama. No hype. Just… cheaper pills and a healthier life. Sometimes the simplest solutions are the ones we ignore.
Sarah Blevins
Correlation ≠ causation. You cite adherence increases after price drops, but fail to control for patient education campaigns, pharmacy outreach, or changes in insurance design. Also, 100,000 preventable deaths? Source? That figure is often misattributed from a 2005 CDC report with a different methodology. Don’t weaponize statistics to push an agenda.
Jason Xin
Oh wow, so now we’re pretending that people who can’t afford insulin are just ‘irresponsible’? That’s rich. Meanwhile, the same pharma execs who price-gouge insulin are flying private jets to Davos to talk about ‘health equity.’ You know what’s worse than high prices? pretending you care while doing nothing. Thanks for the data dump. Now go fix it.
Yanaton Whittaker
YUP. I switched to generic metformin and saved $180/month. I bought a new guitar with that money. My diabetes? Still under control. My mood? Better. My bank account? Thank you, generic drugs. 🙌
Kathleen Riley
It is axiomatic that the commodification of pharmaceuticals, predicated upon the capitalist imperative of surplus-value extraction, fundamentally subverts the ethical foundations of medical practice. The ontological status of the patient, reduced to a mere locus of expenditure, is rendered incommensurable with the moral duty of healing. Hence, the imperative for systemic reconfiguration of pharmaceutical distribution is not merely pragmatic-it is transcendentally exigent.
Beth Cooper
Wait… so you’re telling me the government didn’t want us to know that generics are made in the same factories as brand names? And that the FDA lets the same companies make both? Coincidence? I don’t think so. This is all a scam to make you think you’re saving money when really, you’re just being sold the same pill in a different box. Wake up.
Holly Robin
My cousin’s cousin’s neighbor took a generic and had a stroke. No one talks about that. Why? Because the pharma lobby owns the news. I saw a guy on YouTube say his heart skipped beats after switching. He posted it. Then it got deleted. Coincidence? Nah. This whole thing is rigged. You think your $5 pill is safe? It’s probably filled with talcum powder and corporate lies.
Sazzy De
My doc asked if I could afford my meds last visit. I said no. He handed me a coupon for $0 copay. That’s all it took. No drama. No yelling. Just someone who actually listened. Sometimes care is just… simple.