For millions of low-income Americans on Medicaid, the difference between a generic drug and a brand-name one isn’t just about the label-it’s about whether they can afford to take their medicine at all. In 2023, generics made up 90% of all prescriptions filled through Medicaid, but they accounted for less than 18% of total drug spending. That’s not a coincidence. It’s the result of a system built to stretch limited dollars as far as possible-without sacrificing access.
Why Generics Are the Backbone of Medicaid
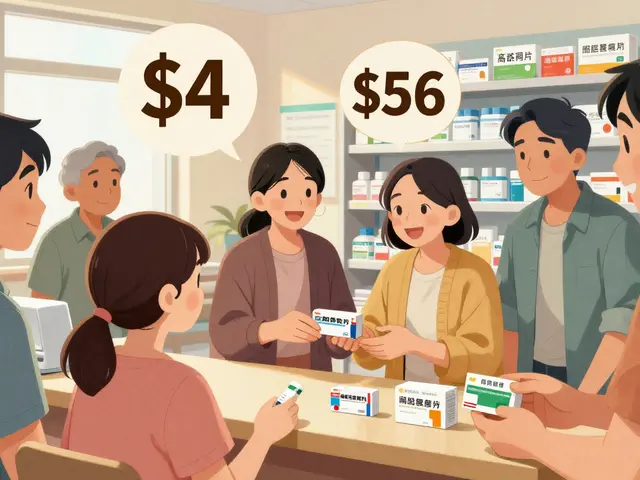
Medicaid doesn’t just cover low-income patients; it has to stretch every dollar to cover as many people as possible. That’s where generics come in. These are exact copies of brand-name drugs, approved by the FDA to work the same way, with the same active ingredients, dosage, and safety profile. The only differences? The name, the color, and the price.On average, a generic drug costs 80-85% less than its brand-name counterpart. For Medicaid, that adds up fast. In 2023, the average copay for a generic prescription was $6.16. For a brand-name drug? $56.12. That’s nearly nine times more. For someone living paycheck to paycheck, that difference means choosing between medicine and groceries.
The system doesn’t stop at just lower prices. The Medicaid Drug Rebate Program (MDRP), created in 1990, forces drug makers to give states a cut of the profit. In 2023, those rebates cut Medicaid’s gross drug spending by $53.7 billion-over half of what was originally paid. That’s money that went back into covering more people, more services, and more prescriptions.
How Much Money Are Patients Really Saving?
Let’s look at real numbers. In 2022, generics saved the U.S. healthcare system $408 billion. Of that, Medicaid accounted for a huge chunk. Here’s why: 93% of all generic prescriptions filled under Medicaid cost less than $20 at the pharmacy counter. Compare that to brand-name drugs, where only 59% fell under that threshold.For a patient with diabetes, switching from a brand-name insulin to a generic version might drop their monthly out-of-pocket cost from $80 to under $10. For someone with high blood pressure, a generic lisinopril can cost as little as $4 for a 30-day supply. These aren’t theoretical savings. These are daily realities.
And it’s not just about the price tag. Lower copays mean better adherence. A Stanford Medicine study found that when patients pay less, they take their meds more consistently. For chronic conditions like asthma, heart disease, or depression, that means fewer hospital visits, fewer emergencies, and better long-term health.
How Medicaid Gets Such Low Prices
Medicaid doesn’t just rely on generics-it actively negotiates. Unlike private insurers, Medicaid has leverage. Because it covers nearly 85 million people, states can demand steep discounts. Manufacturers know that if they don’t offer rebates, they won’t be on the formulary. No formulary = no sales to a huge chunk of the population.For non-specialty generics, Medicaid gets an average rebate of 86% off the retail price. That means if a drug costs $100 at the pharmacy, Medicaid pays $14 after the rebate. And because these drugs are so widely used, manufacturers are willing to accept lower margins to keep volume high.
Even compared to other government programs, Medicaid wins. A 2021 Congressional Budget Office study found Medicaid gets the lowest net prices in the country-even lower than the Department of Veterans Affairs. That’s because Medicaid’s rebate structure is more aggressive than Medicare Part D’s, which had a 86% generic fill rate in 2022 compared to Medicaid’s 90-91%.
Where the System Still Falls Short
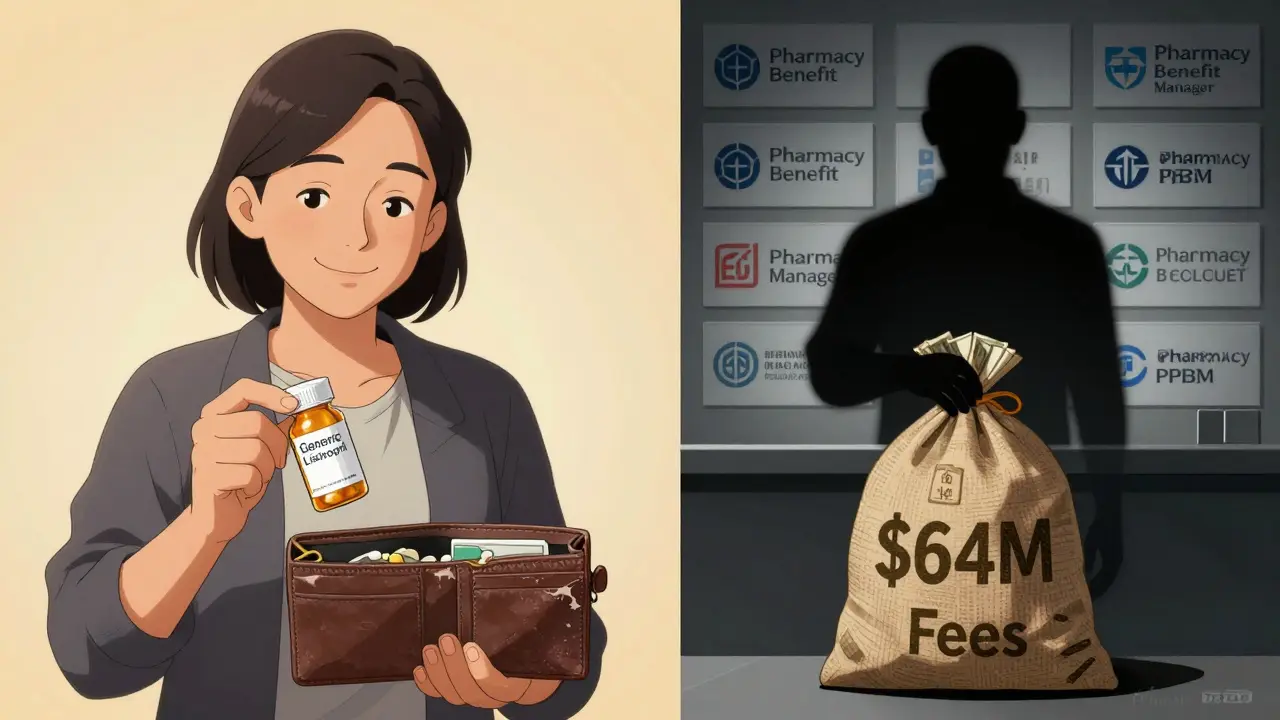
It’s not all perfect. While generics are cheap, patients don’t always see the full benefit. Some states have raised copays for generics over the years, even as drug prices dropped. One patient in Ohio reported her generic asthma inhaler went from $3 to $15 after a formulary change-even though the wholesale price had fallen.Then there’s the Pharmacy Benefit Manager (PBM) problem. PBMs are middlemen between drug makers, insurers, and pharmacies. In 2025, an Ohio audit found PBMs took 31% of the value on $208 million in generic drug sales in just one year. That’s $64 million in fees. That money doesn’t go back to patients or Medicaid-it stays with the middlemen. That’s a hidden leak in the system.
Prior authorization is another barrier. A Reddit user in r/Medicaid shared that her daughter’s generic inhaler cut her copay from $25 to $3-but getting approval took three weeks and six phone calls. For someone without a car, a flexible schedule, or reliable internet, that delay can mean going without medication.

What’s Changing in 2025 and Beyond
Medicaid’s drug spending jumped $10 billion between 2022 and 2024, mostly because of high-cost specialty drugs. These aren’t generics. These are biologics, cancer drugs, and rare disease treatments that cost thousands per dose. Even though they make up less than 2% of prescriptions, they account for over half of Medicaid’s drug spending.To fight back, the Centers for Medicare & Medicaid Services (CMS) launched the GENEROUS Model in 2024. It’s designed to reduce costs by tightening formularies, encouraging generics, and cracking down on unnecessary prescribing. States are also starting to test direct-to-patient pricing models, cutting out PBMs entirely.
Looking ahead, biosimilars-generic versions of biologic drugs-are coming online. Experts predict they could save Medicaid $100 billion a year by 2027. That’s not just a number. It’s thousands of patients who won’t have to choose between rent and their next refill.
What Low-Income Patients Should Know
If you’re on Medicaid, here’s what you need to do:- Always ask if a generic version is available. Pharmacists are required to substitute unless your doctor says no.
- Check your state’s formulary list online. Some states have tiered lists showing which drugs cost $4, $10, or $20.
- Call your pharmacy if your copay suddenly went up. Sometimes it’s a system error, not a price change.
- Use mail-order pharmacies if available. Many states offer 90-day supplies at the same cost as a 30-day retail fill.
- If you’re denied a drug because of prior authorization, ask for help. Many clinics have patient advocates who can file appeals.
Generics aren’t a loophole. They’re the reason millions of low-income Americans can manage their health without going broke. The system isn’t flawless-but it’s working. And with more biosimilars on the horizon, the savings are only going to grow.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict manufacturing standards. The only differences are inactive ingredients like fillers or dyes, which rarely affect how the drug works. Generics are tested for bioequivalence-meaning they deliver the same amount of medicine into your bloodstream at the same rate.
Why do some Medicaid patients pay more for generics than others?
Medicaid is run by states, not the federal government, so rules vary. Some states set fixed copays-like $4 or $6-for all generics. Others use tiered systems where certain generics cost more. Also, managed care plans (MCOs) may have different formularies than traditional fee-for-service Medicaid. If your copay went up, it could be due to a formulary change, not a price increase from the manufacturer.
Can I switch from a brand-name drug to a generic without my doctor’s permission?
In most cases, yes. Pharmacists are legally allowed to substitute a generic unless the prescription says "Do Not Substitute" or the doctor has written "Dispense as Written." If you’re on Medicaid and your prescription is for a brand-name drug, the pharmacist will usually switch you to the generic unless you or your doctor object. Always confirm with your pharmacist if you’re unsure.
Why are some generics not available through Medicaid?
Not all generics are created equal. Some are made by companies that don’t participate in the Medicaid Drug Rebate Program. Others may be new to market and not yet added to state formularies. Sometimes, a brand-name drug still has exclusivity-meaning no generic is legally allowed yet. If a generic isn’t covered, your doctor can file an exception request.
Will the GENEROUS Model affect my access to medications?
The goal of the GENEROUS Model is to lower costs without reducing access. It focuses on encouraging generics, eliminating unnecessary prescriptions, and improving prior authorization processes. In most cases, you’ll still get the same drugs-but the system will work more efficiently. Some patients may see fewer restrictions on generics, while others may need to go through a simpler approval process for higher-cost drugs.



Luke Trouten
Generics aren’t just cheaper-they’re a moral imperative. The FDA’s bioequivalence standards aren’t suggestions; they’re legally binding benchmarks. If a generic doesn’t deliver the same pharmacokinetics as the brand, it doesn’t get approved. Period. The idea that generics are ‘inferior’ is a myth perpetuated by pharmaceutical marketing, not science. We’re not talking about aspirin here-we’re talking about insulin, antihypertensives, antiretrovirals. These aren’t optional. They’re life-or-death. And yet, we still let PBMs siphon off millions while patients wait for prior auths. The system is broken, but the generics? They’re doing their job.
Gabriella Adams
Let me tell you something as someone who’s worked in a community pharmacy for 14 years: the difference between a $6 generic and a $60 brand-name drug isn’t just financial-it’s emotional. I’ve seen people cry because they couldn’t afford their asthma inhaler. Then, after switching to the generic, they came back smiling. One woman told me, ‘I haven’t bought groceries in two weeks, but I took my pills.’ That’s the real impact. Medicaid’s system isn’t perfect, but it’s one of the few things in this country that actually works for people who need it most.
Vamsi Krishna
Look I’m from India where generics are the backbone of healthcare and let me tell you something-Americans don’t even know how lucky they are. In my country, if you want a generic, you have to go to a pharmacy that actually stocks it, and half the time it’s expired or fake. Here? Medicaid forces quality control. FDA oversight. Rebates. Formularies. It’s a miracle. And you’re complaining about $15 inhalers? In Delhi, you’d be paying $200 for the same thing with no insurance. The system is flawed? Sure. But it’s still the most equitable drug access model in the developed world. Stop whining and appreciate the structure.
Brad Ralph
So… generics work. Got it. 🤡
christian jon
THIS IS WHY WE NEED TO CRACK DOWN ON PBMs!!! I’VE SEEN IT WITH MY OWN EYES-MY COUSIN’S GENERIC INSULIN COST $3, BUT THE PBM TOOK $18 IN ‘FEE’ AND THE PHARMACY ONLY GOT $1.50. WHERE DID THE REST GO? NOT TO PATIENTS. NOT TO MEDICAID. TO CORPORATE EXECUTIVES IN NEW YORK WHO DRIVE LAMBOS. AND THEY CALL IT ‘MARKETING SERVICES’-LIKE THAT’S A THING. THIS ISN’T HEALTHCARE. THIS IS A SCAM. WE NEED TO BAN PBMs. FULL STOP. NO MORE MIDDLERS. NO MORE GREED. JUST DRUGS. FOR PEOPLE. NOT PROFITS.
Suzette Smith
Actually, I’ve heard that some generics are made in China and have different fillers. I’m not saying they’re dangerous, but… I wonder if that’s why my cousin’s blood pressure spiked after switching? Just saying.
Autumn Frankart
They’re not telling you the whole story. Did you know that 70% of Medicaid generics are manufactured by companies that also make the brand-name versions? It’s the same factory. Same machines. Same workers. The only difference? The label. And the price. They’re not saving you money-they’re just rebranding the same pill. This whole ‘generics are cheaper’ thing is a marketing ploy to make you feel good while they keep the profits. The real savings? They go to the government’s budget surplus. Not to you.
Skilken Awe
Let’s be real-the GENEROUS Model is just a Band-Aid. You think cutting PBM fees will fix anything? Nah. The real issue is that Medicaid’s formularies are controlled by lobbying groups with ties to CVS, Express Scripts, and McKesson. They write the rules. They set the tiers. They decide which generics get covered. And guess who gets the rebate? Not the state. Not the patient. The middleman. You’re not saving money-you’re just moving the money around the same oligopoly. And don’t even get me started on how they manipulate bioequivalence thresholds to exclude cheaper competitors. This isn’t healthcare. It’s corporate theater.
Steve DESTIVELLE
Generics are not the solution. They are a symptom of a system that has abandoned the human element. We have reduced medicine to a transaction. We have forgotten that healing is not a cost center. The body is not a spreadsheet. The soul is not a line item. When we choose the cheapest pill instead of the most compassionate care, we are not saving money-we are eroding dignity. The real crisis is not the price of insulin-it is the fact that we have accepted this as normal. We have normalized suffering because we are too afraid to ask for better.
Neha Motiwala
Okay but have you considered that some generics are just not as effective? Like I had a friend who took generic sertraline and she said it made her feel like a zombie. Then she switched back to brand-name and she was fine. So what does that say? The FDA says they’re equivalent but people’s bodies are different. And don’t even get me started on how some pharmacies give you the wrong generic because they’re trying to save a few cents. It’s a mess. And the system is designed to make you feel guilty for wanting quality. But you deserve to feel good. Not just alive.
Alyssa Williams
My mom’s on Medicaid and she just switched to mail-order for her generics-30-day supply used to be $6, now 90-day is $12. She’s saving $60 a month. That’s groceries. That’s gas. That’s a haircut so she doesn’t look like a ghost at her grandkid’s recital. And she didn’t even have to call anyone. Just clicked ‘order’ on the portal. The system’s not perfect, but when it works? It’s magic. Don’t let the noise drown out the wins.
Carla McKinney
The data you’re citing is cherry-picked. Yes, generics are cheaper-but you’re ignoring the fact that many are manufactured in facilities with FDA warning letters. In 2023, over 300 generic drug facilities received Class I or II citations. That’s not ‘safe’-that’s a gamble. And the rebate structure? It incentivizes manufacturers to inflate wholesale prices so they can offer bigger rebates. The net result? You’re paying more than you think. The system is a Rube Goldberg machine of perverse incentives. And you’re calling it a victory?
Ojus Save
generics work good i think. my uncle in india uses them all the time and he is fine. also in usa i think its good that medicaid makes them cheap. no need to overthink. just take the pill. its not magic. its science. and its helping people. so good job. :)