Every year, thousands of people in the UK and the US take the wrong medication-or the wrong dose-because the label on their pill bottle was wrong. It’s not rare. It’s not just a glitch. It’s a preventable mistake that happens more often than you think. And the scariest part? You might not know it until it’s too late.
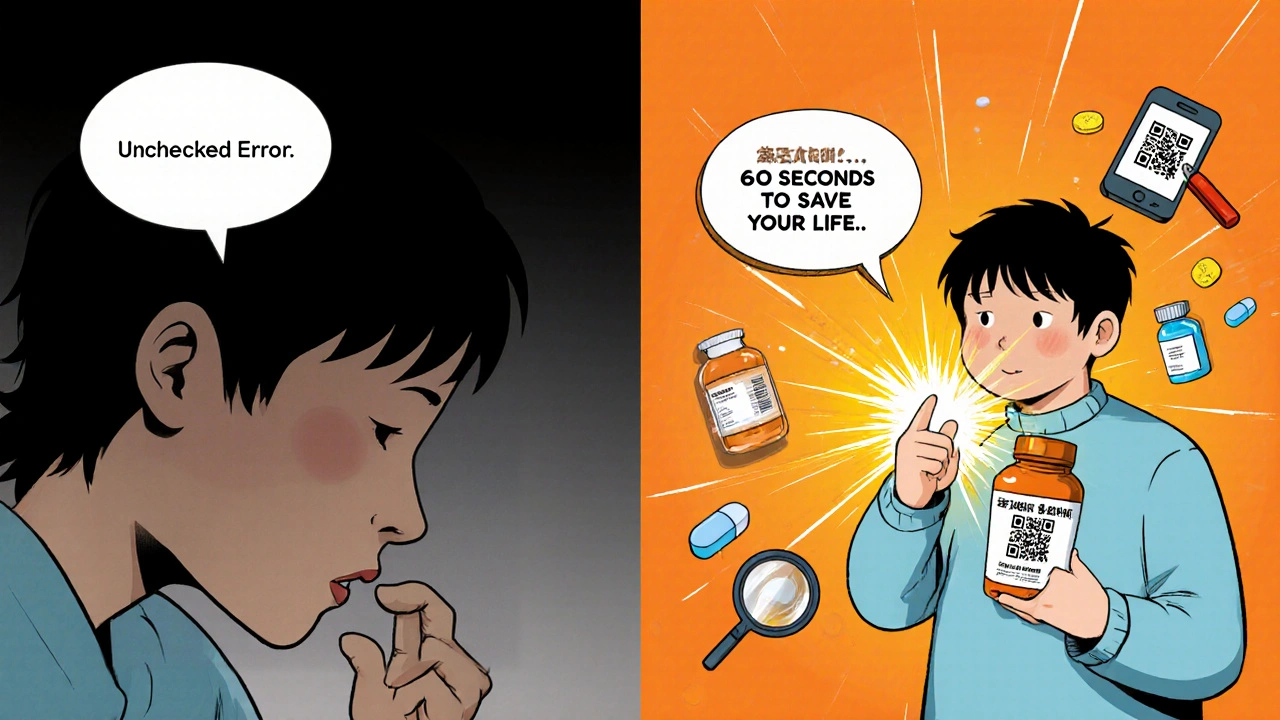
Pharmacies are busy. Pharmacists are overworked. Systems fail. Even with barcode scanners and double-checks, errors slip through. But here’s the good news: you are the last line of defense. Before you swallow that pill, you have about 60 seconds to catch a mistake that could save your life.
What to Check on Every Prescription Label
Don’t just glance at the label. Read it like you’re checking a bank statement. Here’s exactly what to look for:
- Medication name - Both the brand name and the generic name should be clearly printed. If it says “Lipitor” but your doctor prescribed “atorvastatin,” that’s fine-they’re the same. But if it says “Lipitor” and you were supposed to get “Lisinopril,” that’s a red flag.
- Strength - This is where decimal points and zeros cause deadly mistakes. A label that says “5 mg” when it should say “0.5 mg” means you’re taking ten times the dose. Warfarin, insulin, levothyroxine, and opioids are especially dangerous if the strength is wrong. Read the number out loud. Say it. Don’t just look at it.
- Dosage form - Is it a tablet, capsule, liquid, or patch? If you were expecting a pill but got a liquid, ask why. Sometimes the form changes for cost or availability, but you should be told.
- Directions - “Take one by mouth twice daily” is clear. “Take as needed” is vague. If it says “take with food” but your doctor said “on an empty stomach,” that’s a mismatch. Write down what your doctor told you and compare it.
- Indication - This is the reason you’re taking it. Is it for high blood pressure? Depression? Pain? Only 18% of pharmacy labels include this-but they should. If it’s missing, ask for it. Studies show that when patients see the reason on the label, they’re 63% more likely to spot a wrong medication.
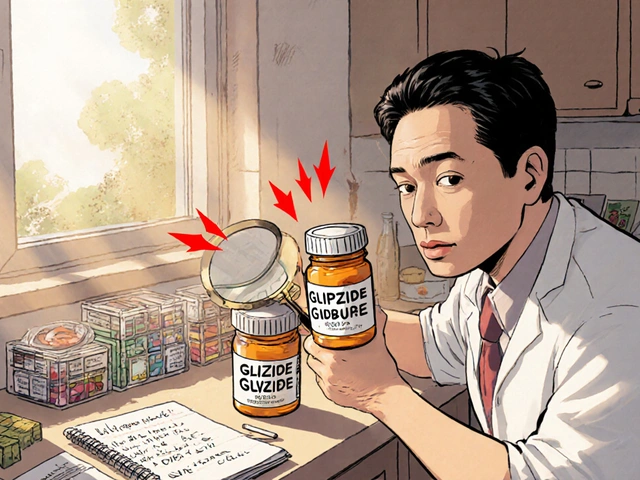
Watch Out for Look-Alike, Sound-Alike Drugs
Some drug names are dangerously similar. It’s not a coincidence. It’s a design flaw.
Take cycloserine and cyclosporine. One treats tuberculosis. The other prevents organ rejection. Mix them up, and someone could die. Or hydralazine (for high blood pressure) and hydroxyzine (for anxiety). One can lower your blood pressure dangerously. The other makes you sleepy.
These are called LASA errors-Look-Alike, Sound-Alike. The FDA tracks over 1,500 of these risky pairs. The fix? Tall-man lettering. That’s when part of the name is capitalized to make the difference obvious. For example: GLIpiZIDE vs. glyBURide. One’s for diabetes. The other? Also for diabetes-but they’re not interchangeable. If you don’t see tall-man lettering on your label, ask the pharmacist if they use it. Most don’t yet.
Compare It to Your Last Bottle
If you’ve taken this medication before, pull out your old bottle. Don’t just remember it-compare it side by side.
Look at the shape, color, size, and imprint code (the letters or numbers on the pill). If your new pills are white and round but last time they were blue and oval, something’s off. Even if the name is right, the pill itself might be wrong.
A 2021 study found that patients who did this simple comparison caught 89% of labeling errors. Those who didn’t? Only 42%. That’s not luck. That’s a system that works.
Ask the Pharmacist: The 4-Step Check
You don’t have to be a doctor to ask smart questions. Use this simple 4-step method, developed by the Agency for Healthcare Research and Quality:
- Compare the label to your doctor’s prescription. Do they match?
- Check the drug name using tall-man lettering if you see it. Is the difference clear?
- Read the strength out loud. Say it. Don’t whisper it.
- Confirm the directions match what your doctor told you.
It takes 90 seconds. And it’s proven to work. In one trial, patients trained in this method caught 92% of fake errors in simulated prescriptions. Those who didn’t? Only 55%.
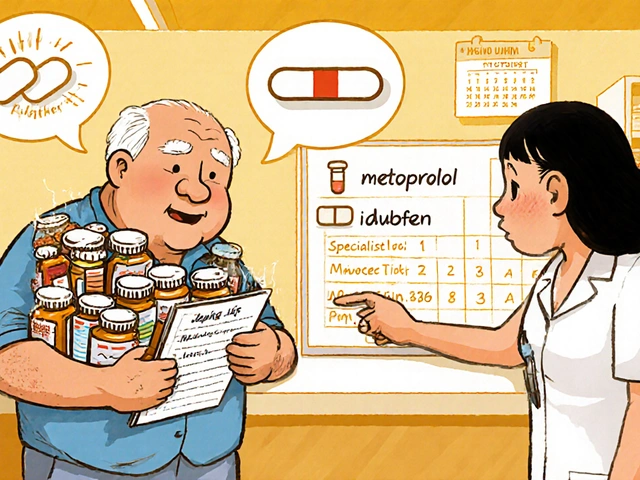
High-Risk Medications Need Extra Care
Some drugs are more dangerous if messed up. These are called “high-alert medications.” If you’re taking one, double-check everything:
- Insulin - A wrong dose can send you into a coma.
- Warfarin - Too much causes internal bleeding. Too little causes clots.
- Opioids - Too much can stop your breathing.
- Chemotherapy drugs - Even small errors can be fatal.
- Anticoagulants (like apixaban or rivaroxaban)
These account for 65% of serious outcomes from labeling errors. If you’re on one, don’t just check once-check every time. And if you’re unsure, call your doctor’s office. They can confirm what was prescribed.
Why People Don’t Check-And Why They Should
Most people don’t check their labels because they trust the pharmacy. That’s understandable. But trust isn’t a safety system. It’s a feeling.
A 2022 survey found that 58% of people who never check their labels say it’s because they “trust the pharmacist.” Another 32% say they just “don’t know what to look for.”
Here’s the truth: pharmacists are human. They make mistakes. A 2020 study found that even with pharmacist double-checks, 3.4% of medication selection errors still get through. That’s one in every 30 prescriptions.
And if you think “it’s never happened to me,” think again. On Reddit’s r/Pharmacy, over 60% of people said they’d personally caught a labeling error in the past year. One woman caught a warfarin dose that was 10 times too high. Another found glipizide instead of glyburide-two different diabetes drugs that caused severe low blood sugar.
What’s Changing to Help You
Things are getting better. New rules are coming.
Starting May 1, 2024, all UK and US pharmacies must use:
- Minimum 12-point font on critical info
- Contrast ratios of at least 4.5:1 (so it’s readable for older eyes)
- Standardized labels that include the reason for use
Apps like MedSafety Check now let you scan your label with your phone and compare it to the correct medication profile. CVS has a feature called “Label Lens” that gives you an audio description of your medicine when you scan a QR code.
But tech won’t fix everything. The biggest barrier isn’t the label-it’s fear. A 2022 study found that 68% of patients who spotted a potential error still took the medicine because they didn’t want to “bother” the pharmacist.
Here’s the truth: pharmacists expect you to ask. They’ve been trained to welcome questions. In fact, Mayo Clinic now requires patients to say back the purpose of their medication before leaving the pharmacy. That’s called “teach-back.” And it cut errors by 68%.
Final Rule: Never Assume
You wouldn’t drive a car without checking the brakes. Don’t take a pill without checking the label.
It’s not about being suspicious. It’s about being smart. You know your body. You know what your doctor told you. The pharmacy is just the middleman.
If something looks wrong, feels wrong, or sounds wrong-stop. Ask. Double-check. Call your doctor. Go back to the pharmacy. It’s your life. No one else is going to protect it better than you.
One extra minute of checking could mean the difference between feeling better-and ending up in the hospital.
What should I do if I find a labeling error on my prescription?
Don’t take the medication. Call the pharmacy immediately and ask them to verify the prescription with your doctor. If they dismiss your concern, call your doctor’s office directly. Keep the label and the pills as evidence. Report the error to your local pharmacy board-this helps improve safety for everyone.
Can I trust the pharmacy if they’ve never made a mistake before?
No. Past accuracy doesn’t guarantee future safety. Pharmacies fill hundreds of prescriptions a day. Fatigue, distractions, and similar-looking drugs can cause errors even at the best-run locations. Checking your label every time is the only reliable way to protect yourself.
Why don’t pharmacy labels always include the reason for the medication?
It’s not required in all places yet, but it should be. Including the indication (like “for high blood pressure” or “for depression”) helps patients catch wrong medications. Studies show this reduces errors by 63%. New regulations in 2024 will require it in most countries, but until then, ask for it.
How do I know if a pill looks different from last time?
Check the shape, color, size, and imprint code (the letters or numbers on the pill). You can look up your medication’s appearance on reliable sites like Drugs.com or Medscape. If it doesn’t match what you’ve taken before, ask the pharmacist if the manufacturer changed. Don’t assume it’s the same.
Are online pharmacies more likely to have labeling errors?
Not necessarily-but they’re harder to verify. If you order from an online pharmacy, make sure it’s licensed and based in your country. Check for a physical address and a licensed pharmacist on staff. Always compare the label to your prescription. If the packaging looks unprofessional or the pills look odd, don’t take them.
Can I use my phone to check if my prescription label is correct?
Yes. Apps like MedSafety Check (launched in 2022) let you scan your label with your phone’s camera. It compares the text to the official drug database and flags mismatches with 94.7% accuracy. Some pharmacies also offer QR codes on prescription bags that link to audio descriptions of your medication. These tools are becoming more common and are worth using.


Josh Gonzales
Been a pharmacy tech for 12 years. The biggest issue isn't the label-it's the handwriting on the script. I've seen '0.5 mg' scribbled like '5 mg' and no one caught it until the patient collapsed. Always read the strength out loud. Seriously. Say it. Even if you're alone in the car.
Ellen Sales
I used to think I was paranoid for checking my pills... until I caught a mislabeled metoprolol that was actually metformin. My blood sugar dropped so fast I thought I was having a stroke. I went back. They apologized. They said 'it happens.' But it shouldn't. You are not being difficult-you're being alive.
Glory Finnegan
Pharmacies are just glorified fast food joints with white coats. They don't care. They're on autopilot. Your life is a speedrun to them. Check your label. Or don't. But don't come crying when your liver turns to mush. 🤷♀️
Oli Jones
In the UK, we’ve had the 'indication' on labels for years. It’s simple. It’s human. It stops people from taking heart meds for anxiety or vice versa. Why is this even a debate? We’re not talking about rocket science-we’re talking about not dying.
Jacqueline Aslet
One must ask: is the act of verifying one's pharmaceutical intake not a metaphysical assertion of autonomy against the bureaucratic machinery of modern healthcare? The label, in its sterile typography, becomes a site of existential resistance-where the individual, armed with nothing but a magnifying glass and a will to live, confronts the indifferent algorithm of corporate medicine. Are we not, in this moment, the last poets of the body?
Caroline Marchetta
Oh, so now we’re supposed to be medical detectives? Because clearly, the $120,000-a-year pharmacist with 37 scripts in front of them doesn’t have time to do their job-so now you, the stressed-out parent working three jobs, are responsible for catching their 0.01% error rate? How generous. Let me just add 'medication safety vigilante' to my 14-hour to-do list. 😌
Valérie Siébert
OMG YES. I just caught my new oxycodone pills were BLUE instead of white. I thought I was going crazy. Called the pharmacy-they said 'oh, different batch!' But I checked Drugs.com and the imprint code was wrong. They had to call my doctor. Turned out it was a mix-up with another patient’s hydrocodone. I saved myself from a nightmare. 🙌 Don’t trust the color. Trust the code.
katia dagenais
Let’s be real-this whole system is designed to fail. You think your pharmacist cares? They’re paid per script. The more they fill, the more they get. The label isn’t broken-it’s *engineered* to be ignored. And now they want you to become a pharmaceutical auditor? This isn’t empowerment. This is exploitation dressed up as education. Wake up. The system doesn’t want you safe. It wants you compliant.
Jack Riley
People say 'trust your pharmacist' like it’s a prayer. But if you trust a mechanic who’s fixed your car 99 times, would you still skip checking the brakes before a highway trip? No. You’d check them anyway. Why? Because trust is not a safety protocol. It’s a luxury. And your life isn’t a luxury. It’s your only currency.
Clarisa Warren
Look I've been to 5 different pharmacies in 3 states and every single one has given me the wrong pill at least once. Not once did they say sorry. They just shrugged and said 'oh, it happens.' So now I bring my own pill organizer and refill everything myself. If you're not willing to do that, don't complain when you end up in ICU.
Dean Pavlovic
Of course you're supposed to check your label. But let's not pretend this is a moral victory. This is capitalism's solution to systemic underfunding: shift the burden onto the patient. You're not a hero for reading the label. You're a victim of a broken system. And the fact that we celebrate this as 'personal responsibility' is the real tragedy.
Austin Doughty
My grandma died because they gave her warfarin instead of lisinopril. She didn't check the label because she trusted them. She was 82. She didn't know what 'atorvastatin' even meant. And now we're telling *everyone* to become pharmacists? That's not prevention. That's cruelty wrapped in a blog post.
Jefriady Dahri
As someone from India where pharmacies often hand out meds without labels, I can say this: if you're in the US or UK and you're being told to check your label, you're already lucky. Don't take this for granted. Do the 90 seconds. It's not hard. It's not your job-it's your right. ❤️
Josh Gonzales
Just saw someone reply saying 'I don't have time.' You don't have time to die either. I've seen 3 people in the last year who didn't check their labels. Two are in the hospital. One is dead. You think you're saving time? You're just delaying the inevitable.